Has malaria finally met its scientific match? Victoria Gill finds out whether a fresh round of research funding could put an end to the killer disease
Has malaria finally met its scientific match? Victoria Gill finds out whether a fresh round of research funding could put an end to the killer disease
When John F Kennedy told the world in 1961 that America would put a man on the Moon by the end of the decade, he triggered one of the biggest scientific and technical projects in history. ’That challenge is one that we are willing to accept, one we are unwilling to postpone, and one which we intend to win,’ he promised in a speech the following year.

Kennedy could easily have been talking about the fight against malaria. Shortly after the second world war ended, global eradication of malaria had seemed to be a realistic goal. Wartime use of DDT had been particularly effective, and policymakers believed that all it would take to stamp out malaria was enough money to supply insecticides and medicine.
It is no small irony that by 1969, when Kennedy’s vision was finally achieved, most public health officials had concluded that the fight to eradicate malaria had largely failed. Indeed, in many regions it had actually strengthened the disease’s grip.
But now there is a renewed sense of optimism and confidence among the scientists, medics and politicians who make it their life’s work to battle the disease. It is bolstered by an enormous fundraising effort from the Global Fund to fight Aids, tuberculosis and malaria; the World Bank; the President’s malaria initiative; and other partners, all of whom coordinate their efforts under the umbrella of the Roll Back Malaria Partnership.
This surge of funding (with particularly heavy-duty support from the Bill and Melinda Gates Foundation) has been a catalyst for action, and success is emerging from its public-private research partnerships - including the first clinically effective malaria vaccine that will enter Phase III trials later this year.
Confidence is so high that Margaret Chan, director-general of the World Health Organization (WHO), now dares to talk about eradicating malaria, rather than merely controlling it. On 14 February the UN appointed a special envoy for malaria, Ray Chambers, a businessman and philanthropist who founded US-based organisation Malaria No More.
He calls the previous lack of emphasis on eradicating malaria a ’genocide of apathy’ and has pledged to raise $8-10 billion (?4-5 billion) over the next four to five years from the ’massive public-private partnership’ that has already started to bear fruit.
Achieving the impossible
Malaria currently kills more than one million people every year - and causes 500 million more to become severely ill. More than 90 per cent of deaths are in sub-Saharan Africa, where malaria kills a child every 30 seconds.

The figures are daunting for anyone hoping to combat the disease. Yet malaria has been eradicated before. From 1945 to 1970, it was driven out of large swathes of East Asia, America, as well as Eastern and Mediterranean Europe.
But during that period, the most vulnerable people in countries worst affected by the disease often had poor access to the drugs and prevention measures they needed, while civil wars and patchy funding also helped to kill off the eradication campaign.
The biggest problem, though, was the fact that the Plasmodium falciparum parasite, responsible for the most common form of malaria, can mutate rapidly to build up resistance to medicines. What’s more, the parasite’s favoured mode of transport - via the Anopheles gambiae mosquito - has also developed its own resistance to insecticides.
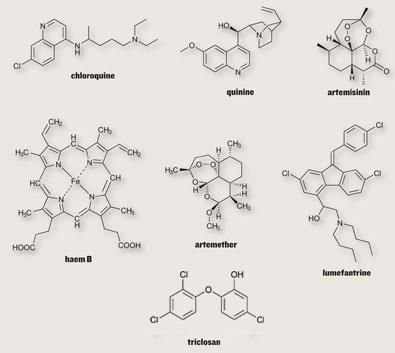
The traditional malaria medicine in Africa had been chloroquine - a cheap, synthetic derivative of quinine, a natural product extracted from the bark of the South American cinchona tree.
Chloroquine blocks the parasite’s ability to digest the host’s red blood cells. As the parasite feeds, it breaks down the oxygen-carrying molecule haemoglobin, releasing the iron-based haem unit. This is toxic to the parasite, which normally polymerises it into harmless haemozoin chains. But chloroquine enters the digestive vacuole of the malaria parasite and caps the haemozoin chains, preventing further polymerisation and causing a build-up of toxic haem that eventually kills the parasite.
However, mutations in the parasite have gradually reduced chloroquine’s ability to create this blockage - a single alteration to a protein that transports chloroquine into the parasite can render the drug useless.
The new gold standard of treatment is now based on another natural product found in Artemisia annua, the Chinese wormwood plant. It has been used for over 2000 years in traditional Chinese medicine, and its active ingredient - artemisinin - was originally extracted and developed into an anti-malarial drug by the Chinese government to protect soldiers during the Vietnam war.
Artemisinin also operates in the parasite’s food vacuole, breaking open its characteristic endoperoxide bridge in a reaction with the iron present in haem and haemozoin.
This reaction releases toxic haem and a burst of free radicals into the parasite. This new mode of action, bypassing changes that have allowed chloroquine resistance to develop, is what makes artemisinin so powerful.
Serious lessons have been learned from past reliance on chloroquine’s single mode of action, and the WHO now endorses the use of artemisinin combination therapies (ACTs) that incorporate several antimalarial agents - hitting multiple targets in the parasite and offsetting the risk of one powerful genetic mutation overcoming the action of a drug.
’Initially none of the big pharmaceutical companies were interested in artemisinin - there was no financial incentive because of where in the world the disease was a threat,’ says Bob Laverty, vice president of communications for Novartis - the Swiss pharmaceutical company that makes Coartem, the most widely-used ACT in Africa. ’But in the 1990s one of the companies that merged to form Novartis approached the Chinese government and expressed an interest.’
The initiative that Novartis has embarked on is one of the many public-private partnerships that have formed the most important part of the global, combined effort against the disease. The financial risk of developing a drug with no significant market is removed by the funding, and companies are gladly offering their best scientists and resources to anti-malarial drug development schemes.
The next generation
The Medicines for Malaria Venture (which gets around 60 per cent of its funding from the Gates Foundation), also based in Switzerland, is one of the non-profit organisations that funds and manages research into new malaria treatments. Its key focus for the immediate future is on new ACTs.
’We work in direct partnerships with drug companies both to develop new drugs and to get them out to patients in the field,’ says Tim Wells, MMV’s chief scientific officer. In early-stage discovery projects, MMV has teamed up with companies including GSK and Novartis to identify compounds in their pipelines that could be developed into anti-malarials.
’ACTs are like anti-malarial grenades,’ says Wells. ’Artemisinin-based drugs are combined with others that have an entirely different mode of action to hit the parasite at multiple targets.’ In Coartem, for example, artemether is combined with lumefantrine, which blocks the haem polymerisation pathway. Lumefantrine is much longer acting than artemether, and provides a back-up - protecting against resurgence of the disease.
’We have four new ACTs coming onto the market in the next couple of years,’ says Wells. ’But we need to be aware of the danger of over-use of artemisinin too - new drugs are always needed.’
One joint project with GSK has discovered that an antibiotic, triclosan, which blocks fatty acid synthesis, a process essential for bacterial growth, can have the same effect in Plasmodium falciparum. In a separate project, GSK/MMV scientists have identified a group of small molecules that inhibit the activity of proteins called falcipains, which also have an essential role in the breakdown of haemoglobin. Wells says that the next generation of anti-malarials could be available by as early as 2015.
Malaria life cycle
Female Anophelesmosquitoes carry malaria parasites in their saliva, which they inject when they bite humans - the saliva also contains an enzyme that prevents blood from clotting, and allows the insect to have a decent meal ( 1 ).
Parasites travel to the human victim’s liver as tiny sporozoites, which invade liver cells ( 2 ). Here they grow and divide, until tens of thousands of daughter cells (merozoites) escape the liver and enter the bloodstream where they invade red blood cells ( 3 ).
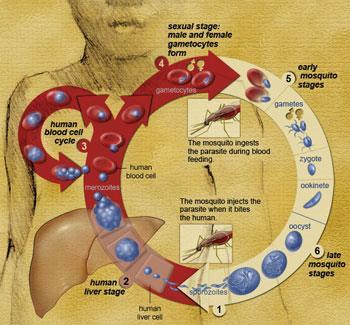
While some of the parasites break down the red blood cells (and are continually released in a cycle of reinvasion), some transform into sexual forms of the parasite, called gametocytes, which are able to reproduce ( 4 ). When a mosquito bites and takes a blood meal from an infected human, it ingests these gametocytes, which mature, reproduce and divide in the mosquito’s gut ( 5 ).
The eventual products of this parasite reproduction are malaria sporozoites, which travel to the mosquito’s salivary glands to start the whole cycle of infection again ( 6 ).
On alert
As new drugs are rolled out, accurate diagnosis of malaria becomes essential in order to avoid prescribing them incorrectly.
Prudence Hamade leads the malaria working group for Switzerland-based M?decins Sans Fronti?res (MSF). In Sierra Leone, she has been involved in MSF’s ’total malaria response unit’ - a pilot project that trains local people to use diagnostic kits, supplies treatments free of charge and distributes insecticide-treated bed nets.
She points out that poorly-organised drug distribution has already caused more long-term problems than it has solved. ’Diagnosis is absolutely fundamental. Because the old anti-malarial drugs were so cheap, they were distributed very freely and administered whenever someone developed malaria symptoms. But the symptoms are so broadly indicative - a fever, headache, flu-like symptoms - that could be caused by a variety of other diseases, such as typhoid. The liberal use of chloroquine has now resulted in widespread drug resistance in the parasite.’
Hamade’s project uses simple diagnostic kits that provide a result within 15 minutes. The tests use a cellulose strip containing a band of antibodies that bind to a malaria biomarker called histidine-rich protein II.
The malaria parasite uses this protein to convert the toxic haem produced as it feeds into harmless haemozoin chains - thus making the protein an excellent indicator of the parasite’s presence, requiring nothing more than a drop of blood and a buffer solution to identify.
According to Hamade, the WHO plans to publish a list of its tried, tested and approved diagnostic tests later this year - enabling healthcare workers to pick the most effective ones from hundreds on the market.
Prevention is cure
A key part of the battle that will take a big step this year is the development of an effective malaria vaccine. Joe Coen, vice-president of R&D on emerging diseases and HIV at GSK Biologicals in Belgium, has spent over a decade formulating the company’s candidate vaccine RTS,S. He calls it his baby. RTS,S uses a section from a protein called circumsprozoite (CSP), which is produced by the malaria parasite and was identified as a vaccine candidate over two decades ago.
Mutation of the parasite is once again a key problem in vaccine design - it is tricky to get the body’s immune system to recognise something that is constantly changing. But the portion of CSP used in this vaccine appears to survive mutations, so the body can be trained to recognise it as the signal for an enemy invasion.
’The original idea was to link the CSP proteins to hepatitis B viral antigen and express the fused genes in yeast cells. They self-assemble into virus-like particles,’ explains Coen. These synthetic viral particles should fool the immune system into responding as if to an infection. ’But the first attempt to develop a vaccine in 1987 failed.’
Coen’s team finally managed to stimulate an immune response with a vital extra ingredient, known as an adjuvant. Immunologic adjuvants have no effect on their own, but are used to enhance the effect of a vaccine - in this case the addition of an aluminium salt made all the difference, although the exact mechanism is unclear. ’The development of a better adjuvant system was the second part of the project,’ says Coen. ’We were able to improve the vaccine and got our first positive clinical result in 1996 - it was a tremendous breakthrough.’
He praises the financial support, particularly of the Gates foundation, for reviving the project. And in Phase II, results have been promising. Importantly, the vaccine appears to be effective in very young children, who are most vulnerable to the disease. The GSK team is now poised for the make or break Phase III trials. ’I now see a light at the end of the tunnel - this is a potentially life-saving vaccine,’ says Coen.
Global malaria
The first spatial map of global malaria risk to be produced in four decades shows that many of the people exposed to malaria are at a lower risk than previously thought.

The Malaria Atlas Project (MAP) found1 that 2.37 billion people are at risk of contracting malaria from Plasmodium falciparum- but about 1 billion of them live under a much lower risk of infection than was assumed by previous historical maps.
’This gives some hope of pursuing malaria elimination because the prevalence isn’t as universally high as many people suppose,’ says David Smith, a University of Florida associate professor of zoology and a co-author of the paper.
Pest control
Where malaria has been successfully eradicated, it has been insecticides rather than medicines that have made the biggest impact. The distribution of insecticide-treated bed nets and indoor spraying is a major preventative approach. In the last three years, washable treated bed nets have become available. Rather than forming a temporary coating on the outside of the net, the insecticide is dispersed throughout the polymer fibres so that it gradually diffuses to the surface and is continuously replaced as the net is washed.
But the mosquito, like the parasite it carries, is not a willing victim - it evolves rapidly to evade such chemical weapons. Hilary Ranson from the Liverpool School of Tropical Medicine, UK explains that there are two kinds of resistance. ’A mutation that changes the target site can disrupt, for example, the binding of the insecticide agent,’ she says. But the parasite can also develop metabolic resistance: ’an up-regulation of the production of enzymes which allows the insect to metabolise the chemical’.
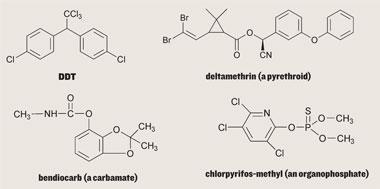
Only four types of insecticide are approved by the WHO for indoor spraying: DDT, pyrethroids, organophosphates and carbamates. All of these target specific proteins essential in the function of the insect’s nervous system - either sodium channel proteins at the membrane between nerve and muscle, or the acetylcholinesterase enzyme that breaks down a key neurotransmitter. These proteins are sufficiently unique to the insect - distinguishable from mammalian proteins - to allow them to be used with a relatively low risk of human nerve damage.
Even so, human toxicity issues mean that of the four types, only pyrethroids can be used in the bed nets themselves. ’You have to assume that babies will be sucking the nets, whereas they’re unlikely to be sucking the walls,’ says Tom McLean, senior executive officer of the Innovative vector control consortium (IVCC), who is also based at the Liverpool School of Tropical Medicine.
The IVCC was set up to address the lack of development of new insecticides against the malaria-carrying mosquito, and received a ?50 million Gates Foundation grant in 2005. ’Half of our grant will be spent on information systems,’ explains McLean. ’We’re developing tools to tell researchers what the insects are resistant to - databases of insecticides, where they are being used and signs of resistance - so that insecticide exposure can be coordinated properly. We’ve also designed lab kits that are in field trials in Africa at the moment, and we will have early versions available this year.’ The kits consist of specific reagents which highlight the DNA markers of resistance.
IVCC is also working with agrochemical companies, including Bayer and Syngenta, to develop new insecticides. ’The public health market is not big enough to support the commercial development of a new insecticide - which from bench to market takes 12-15 years and costs up to $250 million,’ says McLean. ’But if we can absorb the financial risks of development, the companies are more than happy to supply the resources and do the work.’
As well as developing new insecticides from the bench, part of this project involves scouring company pipelines for insecticides that could be used against the mosquitoes, and reviving their development specifically for that purpose. Since many of these chemicals are already registered, and laborious toxicology work has already been carried out, in theory they could be brought onto the public health market within five years.
Supply and demand
One problem with artemisinin combination therapies (ACTs) is that their shelf life can be as little as three years - a major concern when delivering drugs to remote regions lacking fundamental infrastructure is so difficult.

One project based at the University of York in the UK has started to address the issue of artemisinin supply. The university’s Centre for Novel Agricultural Products (CNAP) received a $13.6 million (?7 million) grant from the Gates Foundation for a fast-track breeding research programme for the Artemisia annua plant. The goal is to optimise the plant for high-yielding agricultural production, explains Elspeth Bartlet, a spokesperson from the university. With a combination of genetic screening and selective breeding, the CNAP researchers are rapidly producing plants with bigger leaves and larger leaf glands that contain the vital ingredient.
There have been recent concerns about overproduction of artemisinin threatening the industry (see Chemistry World, January 2008, p6). But Bartlet points out that a balance needs to be struck between supply and demand to make it sustainable. ’This glut will turn into a deficit as more farmers turn away in favour of more profitable crops, such as biofuels. We need to make this crop [Artemisia annua] profitable.’
For the people
Back in Africa, field workers like Hamade and Wells are acutely aware of the gap between major innovative steps in scientific research, and the practicalities of life in a poverty-stricken malaria region.
’People used to reject the bed nets because they found them too hot,’ says Hamade. ’But many people are now finding that they can also help them to get a good night’s sleep, so they are more accepting of them.’ The offer of free bed nets is also used as an incentive to persuade families and pregnant women to attend treatment and infant vaccination clinics. Wells points out that, for children, something as simple as disguising the unpleasant taste of medicines can make a significant difference in how well they stick to their drug regimens - cherry flavour works particularly well.
It’s clear that every piece of this colossal jigsaw counts. Malaria was underestimated once, and the fight against it failed, allowing an even more deadly disease to bounce back. Importantly, the current approach incorporates research projects that will find out if prevention and treatment measures are actually compatible with people’s lives.
The Global Fund’s project aims to halve deaths from tuberculosis and malaria by 2015, and the proof of their strategy will be in those disease’s stark mortality figures. But with a long-term commitment of resources in place, scientists can at least work to arm those on the front line with a fresh set of weapons against malaria.
1 C A Guerraet al. PLoS Med,2008, , e38. DOI:10.1371/journal.pmed.0050038References
1 C A Guerraet al. PLoS Med,2008, 5, e38. DOI:10.1371/journal.pmed.0050038






No comments yet