Stick-on patch with glucose responsive microneedles releases insulin automatically whenever it is needed
With an estimated 387 million people living with diabetes worldwide, research is continually underway to provide better forms of treatment. Now a group of researchers at the University of North Carolina in the US has developed a promising treatment that could automatically dispense insulin to diabetes patients. The team has created patches that release insulin in response to changes in oxygen brought about by high glucose levels and hope this could lead to a smarter, painless way of treating the disease.
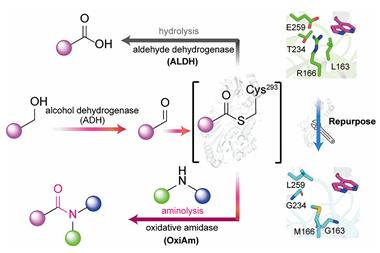
The researchers’ system consists of self-assembled vesicles that encapsulate the enzyme glucose oxidase along with a dose of insulin. Self-assembly is promoted by the vesicle’s building blocks – hydrophilic hyaluronic acid creates an outer shell that protects a hydrophobic nitroimidazole side group.
Under normal physiological conditions the vesicles form a stable system; however, this rapidly breaks down in the presence of plentiful glucose. Glucose oxidase converts excess glucose to gluconic acid, using up oxygen in the process. This lowering of oxygen levels within the vesicle – creating a hypoxic environment – triggers the conversion of the vesicles’ hydrophobic group to a hydrophilic one, causing the vesicle to disassociate and release the trapped insulin.
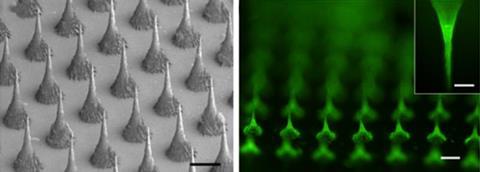
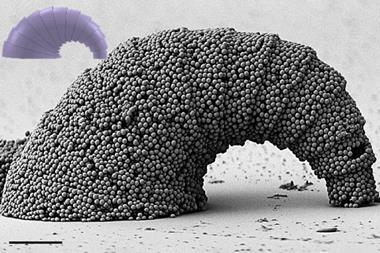
The researchers created a therapeutic patch by embedding the vesicles in biocompatible microneedles, which pierce the skin painlessly when the patch is applied. They tested their patches on diabetic mice and successfully managed their condition for up to nine hours with just one patch.
‘This research is not the first [to look at] glucose responsive insulin delivery,’ says Zhen Gu, one of the researchers at the University of North Carolina. ‘However this is the first time a hypoxia sensitive material has been used to achieve [this].’ Although researchers have exploited the enzymatic conversion of glucose to gluconic acid before, they have mostly used systems that respond to the resulting change in pH. However, pH-responsive systems have much slower response times of around two hours, compared with half an hour for the hypoxia-triggered system.
Robert Langer, an engineer at the Massachusetts Institute of Technology, US, who pioneered the use of polymers to deliver large molecular weight drugs thinks this is very important research. ‘It’s a potentially novel way to treat diabetes,’ he says. ‘It’s a clever piece of work,’ adds Joan Taylor, who researches closed loop systems at De Montfort University in the UK. While she sounds a note of caution about the vesicles potentially being affected by other redox reactions in the body she says ‘the experiment marks a milestone’.
Ultimately, the researchers would like to create a patch that could be used to deliver insulin over two to three days. The treatment is currently limited by the amount of insulin that can be loaded, so they are also investigating using longer or faster acting versions. They now plan to test their patch on micro-pigs, whose skin is a closer match to humans than mice.







No comments yet