A technique to measure how effective chemotherapy is by studying the physical changes that occur in human cells has been developed by US scientists. The method combines atomic force microscopy and Raman spectroscopy to detect biomechanical and biochemical changes in the cells.
The effectiveness of chemotherapy is usually determined by measuring levels of cytokines (cell-signalling proteins) and chemokines (proteins secreted by cells), as well as cell viability, but these traditional methods cannot provide data on single cells, nor do they have the ability to image cells in vitro.
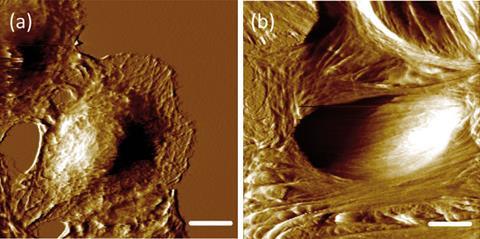
Now, a study by Anhong Zhou from Utah State University and colleagues shows that biomechanical properties can be used to differentiate between benign and cancerous human lung cells. In addition, changes in cellular biomechanics and biochemical components were shown to reflect the different responses of benign and cancerous lung cells to the well-established anticancer drug, doxorubicin. ‘The quantitative analysis of mechanical profiles at the single-cell level can provide additional information that is usually not available in traditional cell biology approaches, but may be crucial to assess and understand tumour prognosis and response to chemotherapy,’ says Zhou.
Atomic force microscopy was used to gather information on cell stiffness by determining the Young’s modulus (stiffness) and adhesion force of the cells. The data were combined with biochemical data from Raman spectroscopy, a molecular vibrational spectroscopic technique that can detect molecular structural information to identify specific (sub)cellular biochemical compositions in living cells.
Hugh Byrne, head of the Focas Research Institute, Ireland, and an expert on the application of spectroscopy for diagnostics and biochemical analysis, thinks such studies are invaluable for evolving Raman spectroscopy for in vitro diagnostic and therapeutic analysis. ‘Increasingly, legislative pressure in the US and EU to minimise the use of animals for scientific research is placing demands on the development of in vitro models for the development of diagnostics and therapeutics,’ he says. However, ‘when establishing these techniques for applications such as routine screening for efficacies of chemotherapeutic or toxic agents and radiation treatments, and even elucidating the mechanisms of action, it is imperative that the techniques be fully validated with model systems and multiple analytical techniques.’
Zhou’s team acknowledges that to better understand how anticancer drug treatments affect the cellular and biomechanical and biochemical responses of human lung cells, more work has to be done in a dose-dependent and time-dependent manner.






No comments yet