Beyond the medical breakthroughs, the hype and the controversy, how are the big drug companies developing their use of stem cells? Sarah Houlton reports
Beyond the medical breakthroughs, the hype and the controversy, how are the big drug companies developing their use of stem cells? Sarah Houlton reports

When a young Colombian woman received the first organ transplant that did not require her to take immunosuppressant drugs for the rest of her life, the potential of stem cells in therapy was finally and dramatically realised. Claudia Castillo, whose respiratory system had been irreparably damaged by tuberculosis, was the first patient to receive a new trachea engineered from her own cells. An international team of scientists stripped the endothelial and cartilage cells from a donor trachea, replacing both with Castillo’s own cells, grown from stem cells taken from her bone marrow. The result? Her body accepted the trachea as if it were her own.
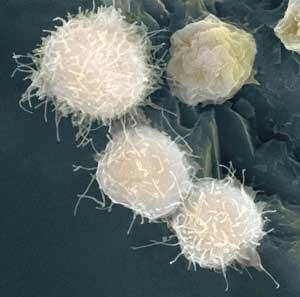
And there are many other ways stem cells could be used in therapy. In theory, stem cells can be programmed to become any type of cell - so it is feasible that they could replace dead cells, and cure otherwise incurable degenerative diseases such as Alzheimer’s and Parkinson’s. They have even been proposed as a possible treatment for paralysis. The fact that it is very early days for stem cell therapies, and that there are many hurdles, both technical and regulatory, has not dampened the hype.
But pharmaceutical companies have even more reason to be interested in these weird and wonderful biological tools. It is likely that the use of stem cells will become routine in drug discovery long before they are commonplace therapeutically.
Become anything
’Biologically, stem cells do one of two things - self-renew to make identical copies of themselves, or differentiate,’ explains Tim Allsopp, chief scientific officer at Stem Cell Sciences, which has a portfolio of technology based on the derivation, growth, manipulation and utilisation of stem cells. There are also different types of stem cell. ’Pluripotent stem cells can differentiate into any type of adult cell, unipotent ones can only become one type of cell, and multipotent stem cells can become one of a limited number of stem cells.’
But working with stem cells can be a political and regulatory headache. In terms of potential therapies, pluripotent human stem cells are the most powerful. But as they are isolated from human embryos there are ethical concerns about their use. The first method for isolating and growing them was developed by James Thomson at the University of Wisconsin, US, in 1998. However, in the past couple of years it has become possible to ’reprogramme’ adult cells into pluripotent cells - induced pluripotent stem cells or iPSs. These were first created from mouse cells by Shinya Yamanaka at Kyoto University, Japan, and a year later both Thomson and Yamanaka published methods for making human iPSs.
’It will take a few years to understand the true strength of the reprogramming technology,’ Allsopp claims. ’Whether it will ever be an underpinning way of generating cells that are good for cell therapy is still an open question - this is dictated by the regulatory authorities.’

In recent years, it has been easier to work with stem cells in the UK than in the US, and Allsopp claims that by setting its regulatory stall out early the UK government facilitated work on the more controversial stem cell types such as human embryonic stem cells (HESCs). Indeed, the Human Fertilisation and Embryology Act, which became law in the UK in November 2008 and will be enacted in October 2009, will make it easier for researchers to develop techniques for stem cell production. Elsewhere in Europe, research has been more difficult, particularly in Germany because of sensitivities about experimentation on humans - although restrictions have now been relaxed - and in Italy because of the predominance of the Catholic church.
In the US the conservative attitude of President George W Bush has meant researchers have only been able to spend government grant money on research using stem cell lines that predate 2001. And this has caused problems. According to Arnold Kriegstein, director of the University of San Francisco’s Institute for Regeneration Medicine, the ruling has, in practice, prevented most researchers from working with HESCs; the permitted cell lines are far from ideal for research, and there are newer, much more stable, lines they would rather use. Fortunately for Kriegstein, as his institute has funding from the Californian state as well as federal National Institutes of Health (NIH) money, researchers there can work with these improved cell lines.
’To comply with NIH regulations, we have to have dual laboratories - with federally funded activities next door to non-federally funded ones,’ he says. ’The work with the non-NIH-approved HESC lines has to be done in areas quarantined from NIH support, using equipment that was purchased privately, and we have to document where everything comes from. It creates a lot of expense.’ But, with the advent of Barack Obama’s administration, he expects these restrictions will be removed, and while there may be no additional funding, the efficiency gained through non-duplication will save them money. ’This will simplify our lives enormously,’ he says.
Testing on stem cells
Pharmaceutical companies are particularly interested in developing stem cell lines as models on which to test drug candidates. Because they have the potential to make better models they should help reduce the drug attrition rate - the rate at which drugs fail during trials. A recently launched initiative in the UK, Stem Cells for Safer Medicines (SC4SM), is an independent, not-for-profit company led by the Association of the British Pharmaceutical Industry (ABPI) and funded by government and pharma companies AstraZeneca, GlaxoSmithKline and Roche. SC4SM’s chief executive, ABPI science and technology director Philip Wright, explains that the company looked at 240 compounds that have failed in clinical trials for safety reasons in the past five or six years, and discovered that, by some margin, the biggest reasons for failure are liver and heart damage.
’If we could reduce attrition by 10 per cent, we think it would save about 7 per cent of the overall cost of drug development,’ he says. Stem cells have great potential in predicting which compounds might have these problems once they reach clinical trials - not least because it is impossible to get sufficient hepatocytes or cardiomyocytes for high-throughput or medium-throughput screening in any other way. ’Many companies were unconvinced by the idea of using differentiated stem cells in early toxicity screening, as they felt the screens that were being suggested were not necessarily better than what they already had, or weren’t aligned with what they needed. We are funding academic groups to develop and, importantly, validate new screens.’
The initial aim is to improve the differentiation of the cells, and develop protocols that could be used across a number of different cell lines. ’The key is actually thinking about what they are going to be used for,’ Wright says. ’In the longer term we want to develop a bank of stem cells, and look at using not just HESCs but also iPSs.’ He believes it will be four or five years before practical screens are ready, but in the longer term it may also be possible to address the issues of long-term toxicity - even 28 day toxicity is currently quite challenging to predict.

GlaxoSmithKline, meanwhile, has entered into a five-year, $25 million (?17 million) collaboration with the Harvard Stem Cell Institute (HSCI). As HSCI’s director Brock Reeve explains, they are starting with a handful of projects in areas such as cardiovascular disease, cancer, neurology and obesity, with further projects to be added in time. ’The projects are headed by scientists on both sides, and coordinated by a steering committee with equal representation from the two,’ he says. ’It’s more than just them giving us money - historically I think that has led to failed relationships between industry and academia.’
The aim is to use stem cells to help discover new medicines, rather than using the stem cells themselves as therapies. ’For example, we are looking for drugs that can stimulate endogenous stem cell replication, or in the neuroscience area we want to develop better assays, creating nerve cells in vitro that could be used to develop more effective small molecules as therapies. The aim is to get cell-based models of disease that will lead us to better therapeutics,’ he says.
Reeve believes the boundaries between academic and industrial research are shifting, and one of HSCI’s aims is to bridge the gap between the two - there are things that each would be unable to do alone. ’GSK has a lot of experience in some disease categories and much deeper chemistry experience than we have,’ he explains. ’If we can discover great targets, they can take them further downstream, with their ability to run large-scale clinical trials and bring products to the market. The commercial sector has chemistry and clinical trials experience, but they don’t have a lot of the deep biology, particularly in the elemental biology field.’
Don’t believe the hype
As therapies in themselves, the work on stem cells is further from fruition. ’Although there is considerable potential in using stem cells and their derivatives such as differentiated cells as therapies, there is currently no way of translating them into a therapy,’ claims Randall Moon of the University of Washington, US. ’It’s more than just the science - unlike making a small molecule into a drug in a factory, there is no model for translating a small dish of cells into something that’s mass-produced, completely uniform and quality-controlled.’
Moon is looking at how stem and progenerative cells are controlled, not only in vitro but also in vivo. ’What are the signalling pathways, what are the cues to which they respond, and what makes them differentiate or proliferate, live or die?’ he says. ’If we understood some of these pathways and cues, then perhaps we could modulate them to some therapeutic end.’ He has shown that it is possible to use a small molecule to activate a signalling pathway in bone marrow transplantation which improves the success rate. ’This proved the concept that we can modulate a signalling pathway in vivo and have an effect on stem cells.’
Moon is now looking at the importance of signalling in other contexts, such as regeneration, and has found there is a tight connection between the activation of signalling and regeneration after injury. ’By understanding the various signalling processes it could be possible to modulate these pathways to achieve some form of therapeutic endpoint,’ he claims.
Realistically, Moon believes that improvements in therapies based on haematopoietic cells - the stem cells found in bone marrow that become blood cells - will be seen soonest. ’After that, one might look forward to anything, given the incredibly unpredictable nature of science.’ he says. ’Maybe the next step for small molecules in stem and progenitor cells will be localised areas such as the spinal cord or bone, but in areas where therapy would be more systemic like Alzheimer’s disease, it might be further out.’

Pfizer is also taking stem cells seriously; indeed, in November 2008 it opened a regenerative medicine unit in Cambridge, UK - it is also active in Cambridge, Massachusetts. Its chief scientific officer Ruth McKernan explains that the company has worked with stem cells for many years in the animal model and screening arenas, but it is now moving on to the stem cells being the target rather than a tool. ’We’re really interested in small molecules that modify cell fate,’ she explains. ’My group is focused on using stem cells as targets for therapeutics, whether small molecules or biologics, and preparing for cell therapy.’
The company believes that having in-house expertise will greatly help it to evaluate external collaborations. And McKernan believes the field is moving incredibly fast. ’There are many publications appearing on the ability of small molecules to control [stem] cell fate,’ she says. ’We have seen small molecules that increase the proficiency or efficiency of making pluripotent cells, and molecules that help direct cells to one fate rather than another. I think all of these are really pharma territory. We have the best collection of small molecules, and if it’s going to help small molecules to help control stem cell differentiation, either for subsequent use in vivo or for making cell therapy, then that’s a great place for pharma to contribute.’
Pfizer is working with stem cells in several therapeutic areas, including diabetes, degenerative diseases and immunology. ’The group in the US will be focused on cardiac and endocrine applications, and in the UK on neural and sensory therapeutic opportunities,’ she says. ’The groups will have a wide array of cell cultures, cell production, cell differentiation and screening technologies, and chemistry, screening and drug metabolism will all be contributed by the mainstream Pfizer organisation. Chemistry will be supported primarily from Sandwich [Pfizer’s UK R&D site] .’
McKernan believes that the opportunity for chemistry in cell therapy is only just being realised. ’In the absence of small molecules or biologics to control cell fate, I think cell therapy would have a much harder job of making a therapeutic. My expectation is that the pivotal piece of science in making therapy viable is the use of small molecules to control the process.’
Sarah Houlton is a freelance science journalist based in London, UK






No comments yet