Using chemistry to treat and prevent abnormal bone growths in military amputees
Researchers in the UK are developing a chemical method to remove or prevent abnormal bone growths in the soft tissue of amputees. They hope the technique will limit additional surgery for seriously injured soldiers.
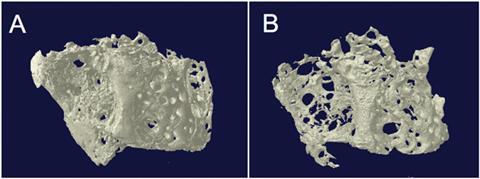
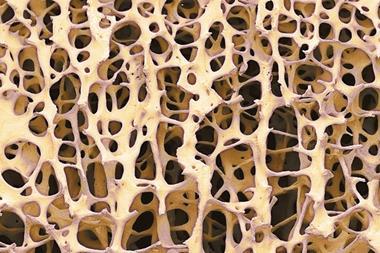
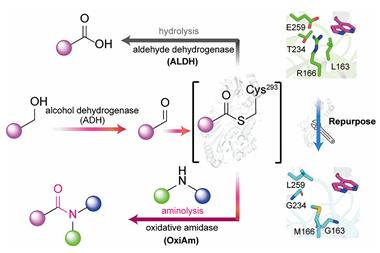
Heterotopic ossification, where a massive inflammatory response causes bone to form within soft tissues, is common in amputees and prevalent amongst combat-injured military personnel. Current treatments targeting the biological pathways involved are limited and surgery is often required to remove the bony growths and ease pain. Now, scientists at the University of Birmingham, including PhD researcher Neil Eisenstein who is also a trauma surgeon in the British Army, are investigating a chemical demineralisation approach using hexametaphosphate as a non-surgical treatment for this debilitating condition.
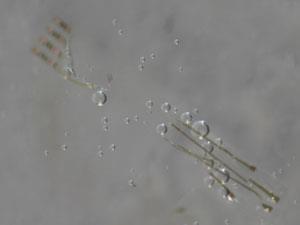
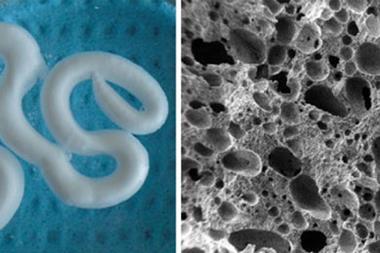
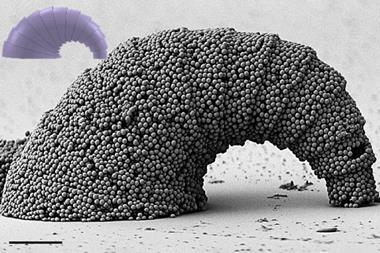
Hexametaphosphate targets hydroxyapatite, the mineral component of bone. Bone incubated in a hexametaphosphate solution for five days showed reduced mass, stiffness and maximum load to failure measurements, indicating that hexametaphosphate dissolved hydroxyapatite. However, quantifying hydroxyapatite dissolution presented a challenge, as Eisenstein explains: ‘Reactions using solid pellets of sintered hydroxyapatite were incredibly slow. To overcome this problem we moved towards using hydroxyapatite sol.’ Interestingly, hexametaphosphate also prevented hydroxyapatite forming when added to an in vitro hydroxyapatite synthesis mixture, suggesting that hexametaphosphate could prevent heterotopic ossification.
Translating this hexametaphosphate-mediated activity into the clinic will not be easy. Iain Gibson, a biomaterials researcher from the University of Aberdeen, UK, describes the main challenge as being able to ‘inhibit formation of heterotopic ossification or demineralise and remove heterotopic ossification [growths], while not affecting healthy bone in the patient’. However, there are promising signs that the team can overcome this particular hurdle. Hexametaphosphate was more effective at dissolving hydroxyapatite at low pH, allowing it to target tissues affected by hypoxia, thought to be a key step in heterotopic ossification bone formation. Hexametaphosphate’s activity can also be inhibited by alkaline phosphatase, an enzyme found in many tissues in the body. These findings suggest that pH or enzymatic regulation could localise hexametaphosphate’s actions.
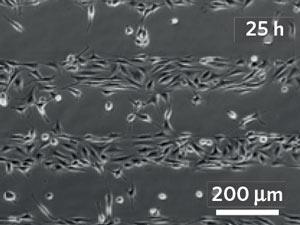
The next step for Eisenstein and his colleagues involves an in vivo model, which brings a new set of challenges. While their in vitro studies suggested collagen was unaffected by hexametaphosphate, the lack of available data makes it hard to predict how hexametaphosphate will behave when applied directly to in vivo tissue. Eisenstein says that future studies will include ‘looking very closely at the soft tissues around the application sites in the modeling stage to ensure that there are no deleterious effects’.
References
This article is free to access unitl 23 June 2016
N Eisenstein et al, J. Mater. Chem. B, 2016, DOI: 10.1039/c6tb00461j






No comments yet