Meera Senthilingam
This week, a compound that caused some disastrous consequences, but thankfully was stopped in its tracks by a puzzle-solving scientist. Explaining more is Simon Cotton.
Simon Cotton
We trust the doctors and nurses who care for us when we are ill. We also have to be able to trust the medications that they provide. This is a story of trust misplaced, of many innocents born handicapped or not even born at all. It is also the story of a remarkable woman, who saved many lives. Her story shows the importance of connecting disconnected facts learned at different times.
Frances Oldham Kelsey was born in Vancouver, Canada, in 1914. She obtained an MSc in pharmacology at McGill University and moved to the University of Chicago in 1937 to study for a PhD. Halfway through her studies, her supervisor asked her to investigate a drug called elixir sulfanilamide, a medication which had caused over 100 deaths, mainly of young children. She established that the cause of the deaths was the toxic solvent that was used, diethylene glycol, and that sulfanilamide itself was quite safe.

After she obtained her PhD, Kelsey joined the university faculty. During world war two, she investigated antimalarial drugs, noting that pregnant rabbits could not metabolise quinine as well as normal rabbits, and rabbit embryos could not break it down at all. She also noted that quinine could cross the placental barrier. She remembered all these facts later when, as a drug reviewer on the staff of the Food & Drug Administration (known as the FDA) in Washington DC, she was asked to review thalidomide.
Thalidomide had first been made in the early 1950s. The West German firm Chemie Gr?nenthal marketed it as an over-the-counter sedative, which unlike barbiturates was not toxic. No prescription from a doctor was needed. Apart from its being a safe sleeping pill, the many uses advised for it included the treatment of morning sickness in pregnant women. As well as its original German market, thalidomide went on to be sold in many other countries, including the UK, much of Europe, Canada and Australia. It had not been available in America when the Richardson-Merrell company filed an application with the FDA on September 12th 1960, to market thalidomide in the United States. Kelsey had 60 days to review the application.
Kelsey was unhappy with the application. The animal safety tests were limited; it had been tried on rats, but not mice or rabbits. There was little clinical evidence and there had been no serious studies of risks to pregnant women. She returned the application to Richardson-Merrell, and asked them for more safety information. In the meanwhile, she saw a letter in the December 31st 1960 issue of the British Medical Journal. An Aberdeen doctor reported that four patients who had taken thalidomide had developed irreversible numbness in the limbs, known as peripheral neuritis. Kelsey asked for more evidence from animal tests, as well as evidence that thalidomide was safe to take during pregnancy.
In the spring of 1961, a young Hamburg lawyer called Karl Schulte-Hillen went to see Professor Widukind Lenz, head of the children's clinic at Hamburg University. His wife Linde had given birth to a son with short, seal-like, arms, a complaint known as phocomelia, which was sadly to become only too familiar. Lenz made enquiries and found 46 mothers of children with such malformed limbs. Nearly all had taken thalidomide. That November he presented his findings at a conference and asked Chemie Gr?nenthal to take the drug off the market (they refused).
His findings made headlines in the German newspaper Welt am Sonntag on Nov. 18, 1961. Almost simultaneously, an Australian obstetrician noted a number of babies born with limb deformities, and whose mothers had taken thalidomide. He reported this in a paper in the Lancet in December 1961. More reports came to light. In the face of the accumulating evidence, thalidomide was withdrawn from the German and Australian markets and on the 8th of March 1962 Richardson-Merrell withdrew their application. Frances Oldham Kelsey's actions meant that thalidomide was never marketed in the USA, saving untold lives.
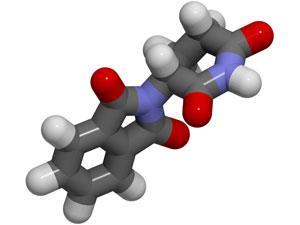
Thalidomide has a chiral carbon atom, so it can form two enantiomers. Both isomers are sedatives, but only one is a teratogen, producing birth defects. It was used as a mixture of the two enantiomers, but even if it had been used as just the 'safe' isomer, birth defects would still have occurred, as the two isomers rapidly interconvert in the body. Thalidomide is believed to have teratogenic effects because it can slide between paired bases in DNA and interfere with the synthesis of integrin proteins. This stops blood vessels forming to supply growing embryonic tissue, therefore some limbs do not grow. Women who have taken thalidomide in the 34-50 day window following the last menstruation are at risk of giving birth to deformed babies. It is at that time that limbs are created in the human foetus, and therefore vulnerable to thalidomide, which causes the death of cells and stops limbs from forming. 5000 babies affected by thalidomide survived childhood but many more died because of the drug.
You, the listener, may have made up your mind about the villains in this story, but there is no doubt about the heroine, Frances Oldham Kelsey.
Meera Senthilingam
Indeed, as her findings prevented even more deaths and deformities in the future. That was Birmingham University's Simon Cotton with the growth-affecting chemistry of thalidomide. Next week, yet another lethal compound.
Neil Withers
Ricin is a highly poisonous natural protein found in the seeds of the castor oil plant. It is thought that the plant makes the poison to ward off predictors because as soon as the seeds germinate, the toxin vanishes.
It is a highly efficient poison, with just a tiny amount needed to kill: 10 castor beans are estimated to contain sufficient ricin to end the life of an average-sized adult. That said, simply swallowing the seeds wouldn't be enough, as the seeds' protective coating would allow them to travel through the gut relatively unscathed. Instead, the ricin needs to be extracted from the seeds, and even then ingestion is a much less effective method than inhalation or injection. If injected, just 200 to 500 micrograms of ricin is enough to kill: an amount small enough to fit on a pin head.
Meera Senthilingam
And discover the chemistry enabling the fatal effects of this compound in only small doses and the dangers of it falling into the wrong hands by joining Neil Withers in next week's Chemistry in its element. Until then, thank you for listening, I'm Meera Senthilingam.






No comments yet