Vitamin D deficiency is on the up. With links to bone diseases and even cancer and MS, we need sun sense, says Justine Davies
Vitamin D deficiency is on the up. With links to bone diseases and even cancer and MS, we need sun sense, says Justine Davies
At this time of year, when the UK languishes in the depths of winter with a dejected sun that barely manages to drag itself over the horizon, thousands of residents cheer themselves up by booking their summer holidays. Meanwhile, Sid the seagull is encouraging Australian citizens to ’slip, slop, slap’ to protect themselves from their scorching summer sun. This campaign to combat skin cancer has been effective in reducing sun exposure in Australia and has also filtered through to other countries, but does reduced sun come at a price?

Sunlight is necessary for the skin to synthesise vitamin D, which is essential for controlling calcium and phosphate metabolism. Without adequate calcium and phosphate to mineralise bone, the skeleton softens and deforms, leading to rickets in children and osteomalacia in adults. Many years ago, when these ’metabolic bone diseases’ were prevalent, vitamin D was recognised to be an important molecule. However, in Western countries, as our diet improved and time spent outdoors increased, they faded into distant memory, along with concerns over vitamin D levels.
Now it seems that metabolic bone diseases are making a comeback. Bill Fraser, a clinical biochemist at the University of Liverpool, UK, is seeing an increasing number of cases, especially in people with low sun exposure. ’In the UK, sunlight is a major determinant of vitamin D and people who spend a lot of time indoors are particularly at risk of deficiency.’ He adds that low vitamin D levels also contribute to the increasing prevalence of fractures related to osteoporosis.
But there is more to the story than metabolic bone disease and some scientists now associate conditions such as multiple sclerosis (MS), some cancers, diabetes, high blood pressure and heart disease with vitamin D deficiency.
Vitamin D’s main job is to maintain blood calcium by increasing calcium absorption from the gut whilst decreasing loss from the kidneys. If vitamin D levels fall, calcium follows and triggers the release of parathyroid hormone (PTH) from the parathyroid glands. PTH also maintains blood calcium levels, but concentrates its efforts on releasing calcium stored in bone. The resulting ’demineralisation’ causes the soft bones of osteomalacia and rickets and contributes to osteoporosis.
Diet doctor
Vitamin D refers to a group of steroid hormones. Vitamin D2 (ergocalciferol) and D3 (cholecalciferol) are the most important for humans. We can get vitamin D2 from our diet - from eating plants and vegetables. Vitamin D3 can be obtained from eating meat, but animals also synthesise their own D3.
The epidermis, or upper layer, of the skin contains 7-dehydrocholesterol, a precursor of cholesterol, which on exposure to ultraviolet (UV) light undergoes a transformation to vitamin D3. This involves a rearrangement of the 5,7-diene in the B-ring which causes a break in the ring to form the 9,10-secosterol, previtamin D3. ’Previtamin D3 is thermodynamically unstable, and it rearranges its double bonds to form the more thermodynamically stable vitamin D3 structure,’ explains Michael Holick of the vitamin D, skin and bone research laboratory at Boston University, US.
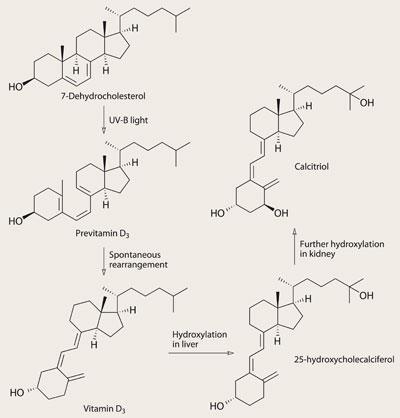
But it doesn’t end there. To produce the calcitriol (1,25-dihydroxy vitamin D3) needed by the body, D3 is transported in the blood stream - on plasma binding proteins - to the liver where it undergoes hydroxylation to 25-hydroxy vitamin D3 and thence to the kidney where it is converted to calcitriol.
D2 undergoes a similar conversion but it is thought to be less biologically active, because it doesn’t stick to the plasma binding proteins as well as D3, explains Fraser. This means that it is not converted in the liver and kidneys as effectively as its counterpart, and is more readily metabolised and excreted.
Although D3 is available in the diet, it is predominantly obtained by synthesis in the skin. In fact, this is so important that, according to Johan Moan of the institute of physics at the University of Oslo, Norway, white skin evolved in the higher latitudes around 5500-10,000 years ago when the onset of farming meant that we no longer obtained enough vitamin D and calcium from our diet. Moan found that ’dark skins reflect more UVB than white skins and do not get enough to synthesise sufficient amounts of vitamin D in winter at high latitudes’.
Modest molecule

Even reptiles sunbathe to top up vitamin D levels, and some of them have got this down to a fine art. Research by Holick has shown that the panther chameleon of Madagascar basks in the sun for just long enough to produce exactly the right amount of vitamin D3. In addition, these chameleons have an interesting dual role for their vitamin D - the males may also use it as a pheromone to signal mating fitness to the females.
And vitamin D may also have other roles in humans. In 1941, says Holick, scientists started to notice that people living at higher latitudes were at a greater risk of death from cancer than people closer to the equator. At the time this was merely an interesting observation, but in the past couple of decades, low levels of vitamin D have been postulated as the link between latitude and cancer. In addition, since the cancer association was discovered, low vitamin D has also been associated with the higher incidence of cardiovascular disease, diabetes, infections and MS found in people at high latitudes.
’Association is the right word,’ says Fraser. There has yet to be any firm evidence that low vitamin D levels cause these diseases, even if the associations are strong.
He argues that the discovery of these associations has a lot to do with our improved ability to measure vitamin D. ’It has become much easier over the last 10 years with the development of automated immunoassays,’ he says.
Still, there is no arguing with the strength of the association. Holick cites a study which reported that ’25 per cent of the deaths due to breast cancer in women in Europe could be attributed to their lack of UVB from exposure to sunlight,’ and another study which demonstrated that men exposed to more sunlight throughout their lives developed prostate cancer three to five years later than men who were not exposed to as much sunlight. Studies have also shown an equally strong association between cardiovascular disease and MS with low vitamin D levels.
Anticancer?
It is still early days in the hunt for an answer to whether low levels of vitamin D actually cause non-bone diseases. But, a number of studies certainly point towards a causal role.
’A number of small randomised controlled trials do show beneficial effects of vitamin D supplementation on blood pressure, blood vessel health and glucose metabolism, says Miles Witham, senior lecturer in ageing and health at the University of Dundee, UK. ’The effects are not seen in all patient groups or all studies, but these initial findings certainly merit further investigation in larger randomised controlled trials.’
There are also possible explanations for the anticancer effects of vitamin D. ’One of the most intriguing, important and unappreciated biological functions of vitamin D is its ability to down-regulate cell growth,’ says Holick. ’Both normal cells and cancer cells that have vitamin D receptors often respond to vitamin D by decreasing their growth.’ It therefore seemed logical that the lower risk of death from cancer in people at the equator was due to exposure to the sun increasing circulating levels of vitamin D.
But there was a problem with this theory. Although scientists knew exposure to sunlight increased levels of calcitriol they also knew that once optimal physiological levels are reached the kidneys will not produce any more. They were left pondering why greater exposure to sunlight had beneficial effects if there was a threshold above which no more vitamin D could be produced.
Then they discovered that prostate cancer cells ’expressed the enzymatic machinery to convert 25(OH)D3 to 1,25(OH)2D3.’ says Holick. ’Since that observation, it has been shown that a wide variety of normal tissues as well as various cancer cells, including colon cancer, breast cancer and lung cancer, all have the ability to make 1,25(OH)2D3.’
So the link between cancer and latitude was found; exposure to sunlight produces the precursors that allow 1,25(OH)2D3 to be produced by cells where it acts locally to regulate growth.
Recent research by Sreeram Ramagopalan and colleagues at the University of Oxford, UK, adds to the evidence that low vitamin D levels cause disease and ’provides more direct support for the already strong epidemiological evidence implicating sunlight and vitamin D in the determination of MS risk’. Ramagopalan found that in people with MS the vitamin D response gene sits right next to a gene strongly linked to MS, called HLA-DRB1*1501. Normally, our thymus gland removes immune cells that are likely to attack our own cells.
But the authors have hypothesised that if vitamin D is in short supply, HLA-DRB1*1501 may not function properly, with the result that some cells escape removal by the thymus and go on to attack the myelin coating of the nerve cells, causing MS.
Take a pill?
If we think that low vitamin D levels cause disease, should we take supplements? This is a difficult question, says Fraser. ’Some countries - like Finland and Sweden - advise that some subgroups, or even the whole population, take vitamin D supplements over the winter. But the guidance in Britain is that we don’t need winter supplements.’ A big problem is that what defines a normal vitamin D level is open to question, adds Fraser. ’Some would say that a level enough to suppress PTH is normal, some would say levels that prevent fractures in studies are normal, and others would go as far as saying that there should be no variation in our vitamin D levels between the seasons.’
Fraser thinks that the British guidance is tantamount to saying: ’it is OK to be deficient in winter, but not the summer.’ However, our ancestors would also have had difficulty in raising their vitamin D levels in the winter. So, have we evolved to cope with this, or has our health remained impaired throughout the millennia because of it?
The other thing to consider is what would be achieved by giving supplements. While Fraser thinks that taking supplements over the winter months may help people who are at risk of metabolic bone disease and osteoporosis, he remains to be convinced that they will benefit people with MS, infections and cardiovascular disease - the diseases for which causation has yet to be firmly proven. Although, at this stage he also admits that there is no concrete evidence that vitamin D supplements are beneficial in people at risk of osteoporosis.
Risk vs benefit
As with all medications the benefits of treatment have to be weighed against the risks. We regulate our own synthesis of vitamin D but no such regulation exists for ingested vitamin D, and taking too much can result in dangerously high calcium levels, leading to kidney damage. For this reason many European countries abandoned the policy of fortifying milk with vitamin D in the 1950s.
There are other, less tangible risks of giving too much vitamin D. Excess calcium can also accumulate in the walls of the coronary arteries, which Fraser says is a known risk factor for heart attacks and angina. In addition, in vitamin D trials for patients with asthma, ’the levels were too high and the symptoms worsened’. So there is a fine line between the risks and benefits of taking vitamin D supplements, which is why Witham is adamant that ’until it is proven in large randomised controlled trials that there are real benefits of vitamin D supplements we should not be giving them as a treatment’.
Peter Ebeling, professor of endocrinology at the University of Melbourne, Australia, has said that children in Australia who were not exposed to a minimum of 25 minutes of midday sunshine, or up to 52 minutes a day before 10am and after 2pm, during their winter were at risk of developing crippling osteoporosis and other bone conditions.
Unfortunately, for people living in the UK, no amount of exposure to our winter sun is going to allow us to synthesise enough vitamin D. However, in the six months of the year when the sun is strong enough to enable manufacture of this essential hormone, surely sensible exposure to the sun can only be a good thing?
Justine Davies is a freelance journalist based in Angus, Scotland
References
M F Holick, Ann. Epidemiol., 2009, 19, 73
A Juzeniene, J. Photochem. Photobiol. B, 2009, 2, 93
K B Karsten et al, Physiol. Biochem. Zool., 2009, 82, 218
W B Grant, Biologic effects of light, 2001, Kluwer
D Bodiwala et al, Cancer Lett., 2003, 192, 145
M F Holick, Am J. Clin. Nutr., 2004, 79, 362
S V Ramagopalan et al , PLoS Genetics , 2009, (DOI: 10.1371/journal.pgen.1000369)






No comments yet