New drug types need careful regulation to reward innovation while protecting patients
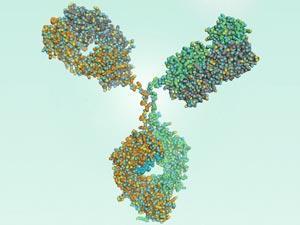
In the last month, three drugs in new therapeutic classes have been approved for cardiovascular diseases. Praluent (alirocumab) from Sanofi and Regeneron, and Amgen’s Repatha (evolocumab), are both antibody drugs that inhibit proprotein convertase subtilisin kexin type 9 (PCSK9) with an aim to lower levels of low density lipoprotein (LDL) cholesterol, which is linked to cardiovascular problems. The two drugs have received complementary blessings from regulators: Repatha is approved in Europe, and recommended for approval in the US, whereas Praluent has won US approval, with a recommendation for approval in Europe.
Novartis’s Entresto (a combination of sacubitril and valsartan) adds a new mechanism of lowering blood pressure relating to heart disease. Sacubitril inhibits neprilysin, which is an enzyme that normally destroys blood pressure-raising peptide hormones (among other peptides). Entresto is now approved in the US and on the fast-track for consideration in Europe.
With such riches on offer, it behoves companies to properly demonstrate the efficacy of their drugs
Heart disease and cholesterol management are high risk, high reward markets for drug companies. They are complex conditions, so the likelihood of failure is significant – particularly when investigating new mechanisms of action. And the efficacy bar is set high by existing drugs: statins for cholesterol, and a raft of blood pressure treatments – many of which are effective and cheaply available as generics. But the prize for a company proving that its drug is better than the competition – enough of an improvement to justify the price of a patented drug over a generic one – is potentially huge, given the global number of patients suffering and dying from cardiovascular diseases every year.
With such riches on offer, it behoves companies to properly demonstrate the efficacy of their drugs – both to regulators and the doctors who will eventually prescribe them (and the organisations that will pay for them). It’s interesting, then, to compare the trial data required for Entresto with that provided for the two PCSK9 inhibitor antibodies.
Entresto’s approval was based on an 8000-patient trial that measured definite clinical outcomes, like cardiovascular-related deaths or hospitalisations for heart failure. It was also compared against a commonly prescribed blood pressure medication, the generic angiotensin-converting enzyme (ACE) inhibitor enalapril. By contrast, Repatha and Praluent have been approved on the basis of sets of smaller trials, demonstrating their ability to lower LDL levels in blood, as measured against placebo, in patients already taking statins. This is a proxy measure, and while there is reasonable evidence that lowering LDL levels has positive health effects, it clearly isn’t the whole story, as clinical failures of other cholesterol-targeting drugs have demonstrated.
To be fair, the regulators have acknowledged this. From the minutes of the US Food and Drug Administration advisory committee’s discussions on these drugs, it’s clear that they considered carefully whether LDL is an acceptable surrogate. Both Praluent and Repatha have only been approved for use in combination with statins, and in relatively limited patient populations – those with a genetic predisposition to high LDL, for whom statins alone don’t lower their cholesterol to acceptable levels, or those who can’t take statins for other reasons. And both Amgen and the Sanofi–Regeneron partnership have larger trials ongoing to try and determine the effect of their drugs on real, clinical outcomes.








No comments yet