After eight years of blaming herself, farmworker Shalan Chinde learned her deteriorating health was not her fault. It began with persistent acid reflux and burning in her chest. Her hands and legs would ache, and some mornings she woke up dizzy and exhausted. The bloating grew worse, followed by pounding headaches, even on days she ate simple home-cooked food.
When she finally underwent medical tests, she was diagnosed with type 2 diabetes. She was determined to find out what was behind this. ‘I live a healthy lifestyle and yet my problems kept piling up each year,’ says the 49-year-old. As the dosage of her medication was increased, she started tracking when her symptoms worsened. On high-pollution days, she noticed her breathlessness increased, her eyes burned, and the acid reflux returned with a painful intensity, triggering headaches that only eased with a painkiller or antacid. When she shared these observations with her doctor, he told her that air pollution was contributing to her symptoms.

For over 15 years, Chinde has been working at a sugarcane nursery in her village in Maharashtra, India. These nurseries have proliferated in the region and the piles of leftover sugar cane stalks that accumulate are frequently burned, sending out thick blankets of smoke.
Chinde’s experience now echoes a growing body of international research, and in a world where the World Health Organization says 99% of people breathe unsafe air, the consequences go far beyond one village. Scientists are finding that air pollution doesn’t stop at the lungs, it can travel deeper into the body and disturb the trillions of bacteria living in the gut.1 These microbes are essential for digestion, metabolism and immunity. When pollution interferes with them, it can trigger biological changes linked to diabetes, obesity, gastrointestinal diseases, cardiovascular conditions and other chronic diseases.
New pathways of harm
Chinde’s story is just one window into a much larger scientific puzzle. Pinpointing air pollution’s impact on the gut is tricky because there are so many variables. But a randomised trial in Uganda offers one of the clearest clues so far. Researchers replaced smoky kerosene lamps with clean solar lamps to reduce air pollution, then collected stool samples before and after the switch to analyse both bacteria and gut viruses.2

They found that the biggest changes were not to the bacteria in the gut but the viruses that infect bacteria and other microbes that live in the gut, called phages. The most substantial shift was in the gut’s virome, the viral ecosystem of an organism, says Peggy Lai at Harvard Medical School, who led the Ugandan study. It showed a broad reorganisation of the phage community after air pollution exposure was reduced. After the switch to solar lamps, the team also saw a rise in helpful, fibre-loving bacteria, linked to producing butyrate, a compound known to calm inflammation. Meanwhile, bacteria associated with inflammation declined.
Women who switched to solar lamps reported fewer breathing problems, although lung function didn’t change over the study period. The takeaway, Lai says, is that cleaner air can help the gut, and a healthier gut may help the lungs.
‘Think of the nose and mouth as two doors leading into the same hallway,’ Lai says. ‘When we breathe polluted air, some of the tiniest particles don’t stay in the lungs; we end up swallowing them. Once those particles reach the gut, they can irritate the gut lining, the protective inner wall of the intestines, and nudge the immune system, thereby shifting which microbes can grow. Even viruses that infect gut bacteria can reshape the microbial balance by killing some bacteria and allowing others to thrive. Together, this can reshape the balance of the gut’s microbial community.’
It doesn’t stop with indoor air pollution. In Italy, higher levels of traffic-related air pollution changed children’s gut bacterial composition.3 Traffic pollutants, including fine particulate matter from vehicle emissions, often mixed with reactive chemicals released by traffic, trigger reactions in the body once inhaled, producing harmful molecules that can damage gut bacteria and disrupt metabolism. While the study didn’t look at disease, the changes it found were similar to those previously linked to metabolic issues.4

Treesa Thomas, an environmental health researcher who has published work on the link between air pollution and disruption of the gut microbiome, explains that pollutants, such as fine dust particles, can cause inflammation and stress throughout the body. Pollution can also weaken the gut’s protective walls, making them ‘leakier’ and allowing harmful substances to slip through.
‘And because the lungs, liver, brain and gut are all connected, pollution can send inflammatory signals or particles to the gut, further disturbing its ecosystem.’ Moreover, pollutants like fine particulate matter, she adds, can shift gut bacteria in ways that interfere with blood sugar regulation, potentially increasing the risk of insulin resistance and diabetes.
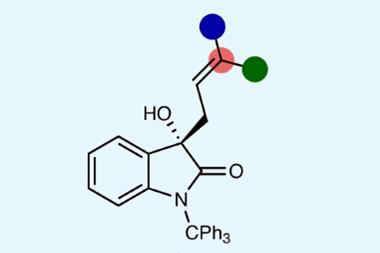
Over the years, many studies have tried to uncover the link between air pollution and metabolic dysfunction. For instance, in China, scientists tracked older adults’ exposure to PM2.5, fine particulate matter less than 2.5μm in diameter that can easily enter the bloodstream.5 They found that higher pollution levels were linked to changes in blood chemistry and higher insulin resistance, an early warning sign for type 2 diabetes.
Worldwide, 2.1 billion people cook using inefficient stoves, leaving households exposed to dangerous levels of air pollution as clean energy sources remain out of reach. Chinde says she has cooked on a traditional stove for over three decades. Aware of the risks, she is taking measures to reduce her exposure and wears a mask whenever she enters areas with severe air pollution.
The unknown health toll
While the links between air pollution and metabolic or respiratory diseases are well established, researchers are now uncovering signs that the effects may go deeper. ‘Altered gut microbes may affect brain function via the gut–brain axis, possibly influencing neurodevelopment or contributing to conditions such as anxiety or cognitive decline, though the evidence here is still early,’ says Thomas. A study of over 1000 older Chinese adults found that long-term exposure to air pollution changed gut microbes in measurable ways. Higher pollution levels were linked to the loss of certain beneficial bacteria, disruptions to microbial energy-metabolism pathways and changes in blood metabolites, which, in turn, were associated with a higher risk of cognitive decline. 6
Moreover, Thomas warns that children exposed to air pollution may experience long-term disruptions in their gut microbiome, potentially increasing the risk for chronic diseases later in life.
‘The firmest take‑home right now is about symptoms; links to specific diseases beyond that are promising but not settled,’ adds Lai.
Even as scientists continue to investigate these links, people like Malan Barwade are dealing with the consequences. For the past eight years, the 60-year-old Maharashtra resident has been struggling with serious acid reflux. She remains so worried about the headache it triggers that she always carries an antacid.
‘I eat home-cooked meals and take care of my health, yet I experience episodes of acidity,’ she says, adding that it gets severe on high-pollution days. Like Chinde, she lives near a sugarcane nursery that sometimes blankets her home in smoke. ‘If you look at the plants near the house, almost all of them have turned grey because of soot,’ she says. With air pollution worsening her health, she was forced to quit farmwork, her only livelihood.

Protecting the gut
Avoiding exposure is rarely an option for people like Chinde and Barwade. ‘We may not always be able to escape polluted air, but there are ways to safeguard or rebalance the gut,’ Thomas says. High-fibre, plant-rich foods feed beneficial gut bacteria, especially the ones that produce short-chain fatty acids, which help reduce inflammation and strengthen the gut barrier. A diverse, plant-based diet can counter the damage caused by pollution. Supplements like probiotics and prebiotics may also help restore microbial diversity. While human studies are limited, she notes, they’re a low-risk option worth considering.
‘The solution is to reduce exposure by switching to cleaner fuels, using air purifiers or avoiding outdoor activity during high-pollution periods,’ Thomas says. She adds that antioxidants, regular physical activity and stress reduction all help maintain the gut’s protective lining and immune balance.

Bo-Yi Yang at Sun Yat-Sen University, China, who has looked at how being outdoors can affect people’s health, says that the exact mechanisms by which green spaces influence the human microbiome remain unclear. However, he says that green spaces might alter the microbiota of the surrounding environment. ‘Trees and grasses may shape the air microbiome by releasing plant particles carrying microbes, secreting volatile organic compounds and changing the microclimate that then influences airborne microbial activities.’
Evidence also suggests that residential greenspace can alter the microbiota in indoor dust, Yang notes. Exposure to greener environments may therefore increase the transfer of environmental microbes into the human body through breathing, skin contact or ingestion.
Greener areas also tend to have lower levels of air pollution, which is known to affect the diversity and abundance of microbes in the human gut. Moreover, many studies have confirmed that regular physical activity can influence intestinal microbial composition and benefit gut metabolism and health.7 Green spaces can encourage physical activity, which itself benefits gut health and alleviates psychological stress, another factor that influences the microbiome.
However, experts say that practical steps alone aren’t enough, as there is still widespread confusion about how pollution interacts with the gut. The most common belief is that pollution affects only the lungs. ‘People assume the gut is protected because it’s internal,’ says Thomas, but inhaled pollutants can move from the lungs into the gut.
Another misconception is that the gut cannot recover once damaged. She points out that the microbiome is remarkably resilient. With a good diet and lifestyle, the gut microbiome can rebalance itself.
For Chinde, the research has offered more context rather than any direct answers. Years of illness left her searching for reasons and, while it is difficult to pinpoint a single cause, science has begun to show how environmental exposures can quietly shape health over time. Today, she tries to be more aware of the air she breathes and adjusts her routine when pollution levels rise. ‘I don’t know what the future holds,’ she says, ‘but I want to stay healthy for as long as I can.’
References
1 X Yu et al, Ecotoxicol. Environ. Saf., 2025, DOI: 10.1016/j.ecoenv.2025.119423
2 C Huang et al, Environ. Health Perspect., 2025, DOI: journal in transition to a new publisher
3 S Filardo, et al, Ecotoxicol. Environ. Saf., 2025, DOI: 10.1016/j.ecoenv.2025.118801
4 T Li et al, The Innovation, 2022, DOI: 10.1016/j.xinn.2022.100213
5 L Zhao et al, Environ. Health Perspect., 2022, DOI: journal in transition to a new publisher
6 W Qi et al, Environ. Health Perspect., 2025, DOI: journal in transition to a new publisher
7 S Varghese et al, Nutrients, 2024, DOI: 10.3390/nu16213663









No comments yet