Curbing industrial practices that drive antimicrobial resistance needs tighter regulation and enforcement
Many of the issues around antimicrobial resistance are compounded by the complex and opaque nature of pharmaceutical supply chains. Most antibiotics are off-patent generics. They are essentially commodities, produced in large volumes with tight profit margins. Those conditions result in significant pressure for manufacturers to reduce costs – all the way from manufacturing and sourcing the various ingredients, to producing finished drugs.
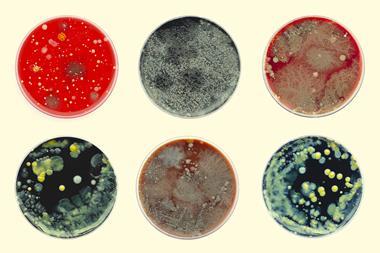
And this is where supply chain opacity brings problems. There are hundreds of manufacturers across the world, from huge multinationals to small and medium enterprises that might make only a handful of products for local markets. Some of those plants operate in areas where stringent regulations are reasonably well enforced. Others are subject to less rigorous oversight. But it’s clear from various investigations that standards vary wildly – whether that’s in terms of the quality of the products themselves and their purity, stability and hygiene, or the associated waste management and environmental protection.
These are not new problems, nor are they restricted to antibiotics, as recent cases in The Gambia, Indonesia and Uzbekistan involving cough syrups contaminated with ethylene glycol and/or diethylene glycol illustrate. While large swathes of the industry operate to high standards, there is a long tail of producers that either can’t, or choose not to, comply with those standards.
Likewise, when it comes to addressing antimicrobial resistance, there are parts of the industry that are making progress across the various issues. Voluntary, industry-led schemes such as external certification through organisations like the AMR Industry Alliance can provide an element of transparency and accountability. But only for those firms that choose to make the effort and investment. Without effective regulation and enforcement, there will always be opportunities for less scrupulous or harder-pressed operators to take the cheaper path to higher profits, regardless of their environmental or public health implications.
Implementing – and then actively enforcing – the controls necessary to curb the environmental and quality failings of antimicrobials’ long manufacturing tail would require a huge injection of resources into regulatory agencies worldwide. It also conflicts with governments’ desire to build on the economic success of their pharmaceutical industries. Prices would almost inevitably rise, and supplies could be disrupted, particularly in low- and middle income countries that tend to rely on the cheapest sources of drugs. These are hard choices to make, but the consequences of inaction are enormous.















No comments yet