India is still waiting for its first fully home grown drug as firm commercialises molecule discovered by charitable venture
Indian pharmaceutical firm Ranbaxy has launched the drug Synriam, which it claims will prove a more efficient and simpler treatment for malaria. It is the first recently developed antimalarial that is not based on artemisinin, one of the most effective treatments for malaria, which has begun to suffer from problems with resistance in recent years. Ranbaxy has hailed Synriam as India’s first domestically developed drug - although none of its active ingredients were discovered in the country.
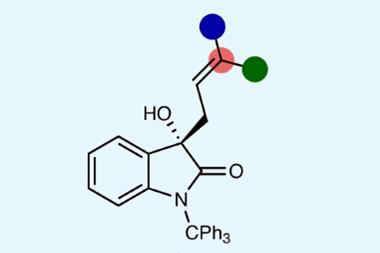
Ranbaxy developed Synriam as a fixed-dose combination of arterolane maleate and piperaquine phosphate, where arterolane is the new chemical entity (NCE) that was developed as an alternative to artemisinin. Synriam was produced as a combination therapy to follow World Health Organization (WHO) guidelines on delaying the appearance of drug resistance. In clinical trials, Ranbaxy reported a cure rate of 95% when three tablets were taken over the course of three days - a simpler drug regimen than other treatments.
According to the WHO, 225 million new malaria cases are reported each year, resulting in more than 650,000 deaths. Most occur in developing countries. With that in mind, arterolane was developed with the goal of creating a drug whose synthesis can be scaled up simply to help keep costs down. By contrast, artemisinin is still produced from plant sources, making it expensive. Arterolane’s simple synthesis process means that it can be sold at less than $3 (£1.85) a course.
Vilasrao Deshmukh, India’s minister for science and technology, congratulated Ranbaxy on the launch of Synriam. ‘I am happy to note that this is first of its kind, a new chemical entity, fully developed through indigenous R&D, which has reached the market,’ he said. However, while much of the global media trumpeted Synriam as the first drug wholly developed in India, Ranbaxy’s press release did not acknowledge the discoverers of the drug.
Arterolane was discovered by a collaborative drug discovery project funded by the Medicines for Malaria Venture (MMV), a Swiss charity. Researchers from the US, UK, Switzerland and Australia, led by Jonathan Vennerstrom of the University of Nebraska Medical Center, US, discovered the intriguing molecule that features an adamantane and an ozonide in its structure.
When it was discovered back in 2003, MMV partnered with Ranbaxy to carry the development through to the clinic. However, after MMV reviewed clinical trial data it backed out from developing the drug further to focus on a derivative of arterolane, which it believed would provide a single-dose treatment for malaria. ‘We collaborated with Ranbaxy until 2007, investing over $20 million in the project,’ says Jaya Banerji, MMV’s director of advocacy and communications. ‘Ranbaxy was [then] granted a worldwide, royalty-free licence for this compound at no cost.’
No Indian pharmaceutical company has solely discovered and developed an NCE-based drug yet. Ravi Raghavan, editor of Chemical Weekly, an Indian trade magazine, says: ‘The price of developing a drug from scratch is a big challenge for Indian pharma because the drug discovery process incurs huge R&D costs and has very low rates of success.’ Indian pharmaceutical industry watchers said that the hype created by Synriam’s launch may hide the fact that since Ranbaxy’s acquisition by Daiichi Sankyo, a Japanese pharmaceutical firm, it has scaled back its drug discovery efforts. Daiichi Sankyo bought a majority stake in Ranbaxy for $4.6 billion in 2008 with the aim of establishing a dominant position in the global generic drugs market.
Ranbaxy now hopes to introduce Synriam to other malaria endemic countries in Africa, Asia and South America. With its affordable price and high efficacy, Synriam may well be a step towards achieving the WHO’s goal of eradicating malaria by 2050, but Ranbaxy cannot take all the credit for it.
Akshat Rathi










No comments yet