Scientific and regulatory progress is helping minimise the impact of mutagenic impurities
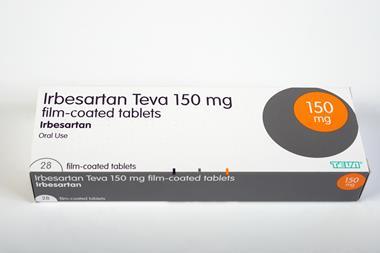
In June 2018, a potentially carcinogenic nitrosamine impurity, N-nitrosodimethylamine (NDMA), was detected in valsartan, a medication used to treat high blood pressure and heart failure. Soon after, NDMA and further small dialkyl N-nitrosamine impurities were discovered in other sartan active pharmaceutical ingredients (APIs), and later in stomach acid regulator ranitidine, and diabetes medicines piaglitazone and metformin.
‘At that time, the risk was related to the manufacture of the drug substance,’ explains Andrew Teasdale, senior principal scientist in impurity management at AstraZeneca. ‘In the case of valsartan it was due to an issue with the chemistry; they had an impurity that was a secondary amine, and they had a nitrosating agent – sodium nitrite – that was used as a quenching agent. And completely by accident, they created this nightmare scenario.’

Since then, comprehensive assessments have been carried out on APIs, drug products and packaging to understand and evaluate the context and extent of the risk of nitrosamine formation. ‘After about three years or so, we thought we were pretty close to solving the whole problem…we thought we understood the chemistry,’ Teasdale continues.
But, it slowly became apparent that the drugs themselves could pose a potential risk. ‘If the drug itself was a secondary amine, particularly if you’re using processes like wet granulation where you’ve got a fair amount of water present, you can dissolve the trace nitrite that’s commonly present in [other ingredients of the formulation] in the water…and again, you’ve got the chemistry conditions to form a nitrosamine.’
All of a sudden there was a major risk of having to take 20%, 30%, even 40% of all existing drugs off the market
The problem with these more complex nitrosamines, referred to as nitrosamine drug-substance-related impurities (NDSRIs), is there is little to no safety data available. That makes it very difficult to confidently set an acceptable intake limit, which is calculated by assuming a lifelong daily exposure to the medicinal product.
Initially, medicines regulators applied the same precautionary limits for the NDSRIs as they had previously for the simpler dialkyl nitrosamines of 18ng/per day. But these were considered unachievable for the NDSRIs. ‘There’s no realistic chance of ever being able to hit limits like 18ng/day,’ explains Teasdale. ‘So, all of a sudden [for maybe] 20%, 30%, even 40% of all existing drugs across major classes – hydrochlorothiazide, beta blockers etc, there is a major risk of having to take these drugs off the market.’
The pharmaceutical industry sprang into action to develop a greater understanding of the likely carcinogenic potency for different NDSRIs. Was it was possible, in the absence of any safety data, to bracket the NDSRIs into different potency groups? Regulators also made various attempts to come up with interim intake limits, but the problem was more serious than anyone had expected. ‘We seemed to be heading towards a catastrophic loss of critical medicines,’ recalls Teasdale.
Regulatory review
In September 2019, the European Medicines Agency (EMA), US Food and Drug Administration (FDA) and regulators around the world asked companies to carry out a comprehensive review of all chemical and biological human medicines for the possible presence of nitrosamines, with an initial risk evaluation due by 1 July 2021 and full confirmatory testing by 26 September 2022.
Those that found products containing nitrosamines above a certain level were asked to submit any relevant changes to manufacturing processes, formulation or packaging – intended to prevent or minimise the risk of impurities forming – to their respective regulators by 1 October 2023.
Speaking to Chemistry World in August, a spokesperson for the EMA said that for centrally authorised medicines, the global response rate for the risk evaluation to identify active substances and finished products at risk of N-nitrosamine formation or cross-contamination had exceeded 96%.
Overall, a risk has been identified for 17% of chemical products. Upon testing, 15% of those (around 2.5% of total products assessed) have, so far, been identified as containing nitrosamines above the relevant limits.
The EMA guideline on assessing and controlling mutagenic impurities states that the first step is an in silico assessment. NDSRIs and other nitrosamine impurities will typically trigger an alert for mutagenicity and be categorised as class 3 impurities, which means there is a structural alert, but no mutagenicity data. This class can generally be controlled either at or below the threshold of toxicology concern, or an Ames test can be conducted to confirm or disprove potential mutagenicity.
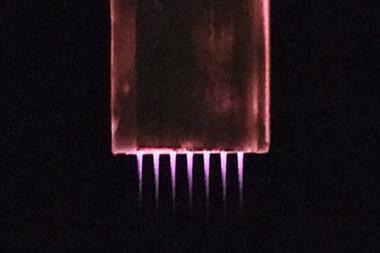
The Ames test is a bacterial reverse mutagenicity test. It starts by incubating bacteria that require, but are incapable of synthesising, the amino acid histidine. ‘Some of the bacteria ‘back-mutate’, so that they will be able to synthesise the amino acid. And if you have a mutagenic substance that you mix with the bacteria, the mutation frequency may increase, so more bacteria will be capable of building colonies,’ explains Joerg Schlingemann, principal expert for quality control systems at Merck KGaA Healthcare.
The Ames test is positive if there is a significant increase in the number of colonies when the bacteria is mixed with the potential mutagen, compared to the non-mutagen or the negative control. For most drug impurities, a negative Ames strongly suggests the compound would not be carcinogenic. They would then be classified as class 5 non-mutagenic impurities and are subject to less stringent concentration limits.
However, because of the heightened concern around nitrosamines, a negative Ames test on its own is not enough to disprove mutagenicity. At the beginning of 2022, authorities raised concern over the validity of Ames results for nitrosamines on the basis that the optimal conditions for detecting mutagenic nitrosamines in the Ames test had not yet been fully determined. The mutagenic potencies of nitrosamines could differ significantly and did not correlate to similar carcinogenic potency.
Since the initial call for review, scientific understanding of nitrosamine impurities, and how to calculate acceptable intake limits, has advanced dramatically.
Game changer
In July, the EMA and FDA updated their guidance on nitrosamine impurities, to include the Carcinogenic Potency Categorization Approach (CPCA) for assigning intake limits in cases where there isn’t enough direct mutagenicity data. ‘For a lot of our existing drugs, it makes a huge difference,’ explains Teasdale.
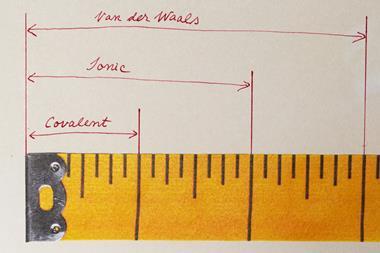
The CPCA assumes that α-hydroxylated derivatives of nitrosamines are responsible for most of the mutagenicity and carcinogenicity. These can form during the body’s attempts to metabolise the compounds, when liver enzymes oxidise the carbon adjacent to the nitrosamine group to an alcohol.
There are reasonably well-understood structural features that directly increase or decrease the favourability of this activation mechanism, as well as features that can speed up the removal of a nitrosamine by other biological pathways. Therefore, the CPCA is based on the idea that, in the absence of sufficient substance-specific data to derive an accurate intake limit, a prediction of the mutagenic potential and carcinogenic potency of an N-nitrosamine can be generated based on the structural features.
In addition, the updated guidelines include details of an ‘enhanced’ Ames test which requires two nitrosamine positive controls that are known to be mutagenic. Since it is the metabolic products of nitrosamines that are mutagenic, rather than the nitrosamines themselves, the revised test also includes metabolic enzymes to activate them.
Evaluation of this enhanced test is ongoing, says Teasdale. ‘There are concerns about whether it’s overly sensitive,’ he explains. ‘Do we really need two positive controls? And what should they be?’
Difference in opinion
The majority of API-derived nitrosamines will probably fall into CPCA potency category 5, says Schlingemann, meaning they would need to be controlled to a limit of 1500ng/day. While he says this is ‘rather easy going’ for most drug products, it does mean that the nitrosamine is still being recognised as a mutagenic impurity.
‘If you want to control it as a non-mutagenic substance you have to perform in vivo mutagenicity testing,’ says Schlingemann. ‘Either a transgenic rodent assay, or there’s a new kid on the block called duplex sequencing.’ Although Teasdale highlights that there are some grey areas and differences in opinion between the regulators in this regard. While in Europe, a negative transgenic rodent assay might be enough to classify a drug as non-mutagenic, ‘the FDA isn’t saying that,’ he says.
Even for compounds still classed as mutagenic, there are differences, he points out. ‘As far as Europe is concerned, if I do this revised Ames test and I get a negative, I’ve got a fighting chance of control, as I can apply a limit of 1500ng/day,’ explains Teasdale. ‘As far as the FDA is concerned, they’re not prepared to go as far as saying a negative Ames will take you to that limit.’
In cases where nitrosamine levels can’t be controlled to below the relevant limit, manufacturers will need to implement technical mitigations. This could involve finding additives that help to control low levels of nitrite, or it may mean changing the packaging or reducing the shelf life of the drug.
Theoretically, manufacturers could change the formulation of affected drugs to include nitrosamine scavengers such as ascorbic acid, but any change to the formulation will lead to regulatory complexities as additional stability studies may be needed and the resulting approval process could take years.
A helping hand
Ultimately, all manufacturers will have to demonstrate to the regulators that they understand where all the nitrosamine impurities are, exactly how they are formed and how to control them. However, while some sources of nitrosamine impurities are relatively easy to identify, others that arise during the various stages of making a finished drug can be harder to identify.
Lhasa, a not-for-profit organisation in Leeds, UK, that facilitates collaborative data-sharing projects in the pharmaceutical, cosmetics and chemical industries, has built software to help model and predict potential sources of mutagenic impurities, in a way that is consistent across manufacturers and reassures the regulators that the calculations have been done properly.
Your stomach is an incredible reaction vessel, full of nitrites from our natural environment. You will generate these chemicals anyway that you can’t control
Lhasa acts as an ‘honest broker’ with whom companies can share unblinded data, while preserving their intellectual property. Lhasa can then learn from the data and use it to create algorithms that everyone can benefit from.
‘The problem with nitrosamines is that the levels that they have to be controlled to are so super low that proving a negative is, in many cases, beyond the capability of the testing technology at present,’ explains Michael Burns, principal scientist at Lhasa.
The function of the software is to highlight to manufacturers when the various factors combine that could give rise to an important impurity, Burns says. ‘Then it’s up to them to assess that risk.’
But this is a huge job, Burns explains, because if you’ve got any secondary amine of any description in your product, it could form a nitrosamine, and secondary amines are everywhere: in drugs but also in food and in our bodies.
‘This is part of the context that can get lost with the focus on the pharmaceutical world – that your stomach is an incredible reaction vessel, which is full of nitrites from our natural environment,’ Burns says. ‘It’s very acidic, which is prime conditions for any amines in your stomach, you will generate absolutely tonnes of these chemicals anyway that you can’t control.’
The science in this area has evolved rapidly
The guideline for most drugs allow for cases where a patient is only going to be taking them short term, meaning intake limits can be higher. But at present, this is not being allowed for drugs containing nitrosamines, says Burns, ‘which negates the fact that we know there are repair mechanisms in the body to redirect all of this because it deals with it daily’.
However, Burns is positive about the progress that has been made since the review started and says that industry and regulators now know much more about the toxicology of nitrosamines than they did before.
Another positive has been in seeing regulators and industry working together to find a solution. As an intermediate between industry and the regulators, Burns has been involved in a lot of meetings with both. Although he says at first they were ‘at loggerheads’, with the regulators being ‘too cautious’, a focus on collaboration has resulted in them being in a ‘much better place’.

‘The regulators have now reached a point where they have been happy setting some higher limits for certain classes, based on what we know about metabolism; ie that it’s not the nitrosamine itself that is mutagenic, it’s once it’s metabolised.’
And Lhasa’s software will continue to develop: ‘the better the information that gets put into the software, the better the predictions come out’, says Burns.
A long road ahead
But there is still a long way to go; industry is still collecting data about the mutagenicity and carcinogenicity of nitrosamines and, with each day, more is understood about how they form.
‘The science in this area has evolved rapidly,’ says Teasdale. ‘For example, we’ve shown that, in the solid phase, in a tablet, tertiary amines really aren’t much of a risk.’ That immediately brings down the proportion of drug products that are likely to be affected. ‘And the CPCA takes it down another notch.’
But Teasdale believes that the ongoing difference in opinion between the regulators will have an impact on progress. ‘The FDA is still concerned about the correlation between mutagenicity and carcinogenicity in the case of nitrosamines, and therefore it’s difficult to work out how to move them from their current position to the position of Europe. That’s the real challenge,’ he says. ‘If you’re ever going to turn this into a business-as-usual activity that becomes just part of the norm, these things still need to be resolved.’
References
1. R Nudelman et al, Org. Process Res. Dev., 2023, DOI: 10.1021/acs.oprd.3c00100
2. I W Ashworth et al, Org. Process Res. Dev., 2023, DOI: 10.1021/acs.oprd.2c00366
3. R C Cioc et al, Org. Process Res. Dev., 2023, DOI: 10.1021/acs.oprd.3c00153
4. N S Murphy et al, Org. Process Res. Dev., 2023, DOI: 10.1021/acs.oprd.3c00118
5. I W Ashworth et al, Org. Process Res. Dev., 2023, DOI: 10.1021/acs.oprd.3c00084
6. I W Ashworth et al, Org. Process Res. Dev., 2023, DOI: 10.1021/acs.oprd.3c00073
7. D J Ponting and R S Foster, Org. Process Res. Dev., 2023, DOI: 10.1021/acs.oprd.3c00008
8. F J King, A D Searle and M W Urquhart, Org. Process Res. Dev., 2020, 24, 2915 (DOI: 10.1021/acs.oprd.0c00462)


















1 Reader's comment