Lithium deficiency in the brain could be an underlying contributor to Alzheimer’s disease, according to new research led by scientists at Harvard Medical School in Boston, US. The findings suggest that it may be possible in future to stall or reverse the disease by administering lithium, though this has not yet been shown in patients.
Harvard neuroscientist Bruce Yankner initially noted that giving high concentrations of lithium dampened signs of Alzheimer’s in mice. His team then measured levels of various metals in post-mortem brains of participants in the Religious Orders Study, a long-running medical study involving Catholic nuns, priests and brothers aged 65 year and older. Of 26 metals, only lithium was significantly reduced in those with mild-cognitive impairment, a forerunner of Alzheimer’s disease.1
Abundance of zinc was higher and copper lower in those with Alzheimer’s, agreeing with previous reports. However, Yankner notes that ‘by far the most significant alteration was in the reduction of lithium in the Alzheimer’s patients’.
Lithium has previously been proposed as an Alzheimer’s treatment, while a 2017 nationwide study in Denmark reported a link between higher levels of lithium in drinking water and a lower incidence of dementia.
After their initial observations, Yankner’s team fed both healthy mice and mice with Alzheimer’s-linked genetic mutations a diet 90% reduced in lithium, which cut levels in their blood by 90%. Their brains nevertheless retained lithium at 50% the levels of mice fed a normal diet.
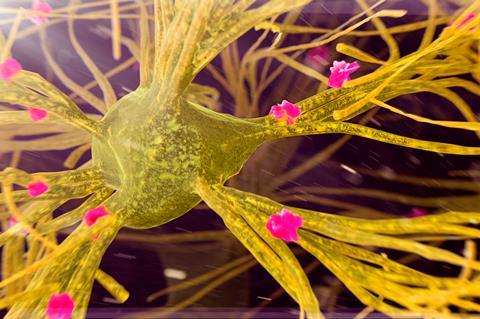
This halving of lithium in the mouse brain boosted the formation of amyloid plaques, tangles of tau protein and pro-inflammatory signals from brain immune cells, all of which are considered hallmarks of Alzheimer’s disease. In turn, this speeded up the loss of brain connections and cognitive decline.
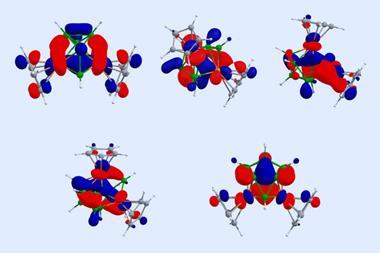
RNA sequencing analysis revealed that gene expression was changed in multiple brain cell types when lithium was deficient. The researchers suggest that this is partly due to lithium’s natural role in blocking an enzyme called GSK3b, dysregulation of which has been linked to Alzheimer’s.
The team also noted that lithium levels were higher in amyloid plaques than nearby regions, suggesting that a build-up of plaques traps more lithium. They suggest that a shortage of lithium could weaken the ability of specialised immune cells called microglia to clear amyloid, while more amyloid traps more endogenous lithium and exacerbates the deficiency.
‘It was intriguing how widespread the effects of lithium deficiency are – on amyloid, tau tangles, [the nerve insulator] myelin, inflammation and a loss of synapses and axons,’ says Yankner. ‘This is a potential mechanism for multi-system degeneration that gives rise to dementia.’
Restoring function
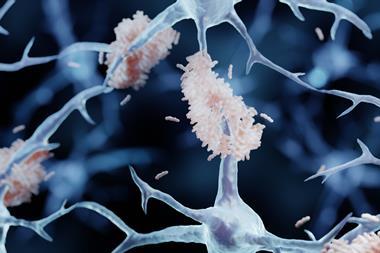
Yankner’s team tested 16 lithium salts for their propensity to become trapped in amyloid plaques. They found that lithium carbonate, which is currently used in the treatment of mood disorders, was easily trapped within the positively-charged plaques. Lithium orotate had the lowest affinity for amyloid, and further tests in mice showed promise. ‘Microglia from lithium-deficient mice were impaired in their ability to degrade amyloid-beta peptide,’ says Yankner. ‘When the mice were treated with lithium orotate, they had that ability restored. It was quite impressive.’
The team now hope to move towards a clinical trial with a lithium salt that can steer clear of amyloid plaques and be easily administered. However, Yankner cautions that nobody should take lithium based on this study, until it is proven in human trials. While lithium-based medicines can be taken safely at prescribed doses, at high levels lithium can be toxic, potentially causing intestinal and neurological symptoms.
Serge Gauthier, a neurologist at McGill University in Montreal, Canada, describes the findings as ‘spectacular’. ‘The potential of low supplemental doses of lithium has been suggested in the past,’ he notes. Gautier says that he is not aware of a reduced incidence of Alzheimer’s in long-term lithium users, but notes that people with bipolar disorder are often excluded from Alzheimer’s research.
‘These are some of the most compelling data yet that lithium is a physiological signalling ion, rather than an irrelevant trace metal that is only important as a drug,’ says Ashley Bush, a neuroscientist at the University of Melbourne, Australia, who has written a separate commentary on the new research in Nature.2 He notes that in addition to GSK3b, ‘it is likely that there are further biochemical targets whose activities or interactions might be modulated by lithium’.
According to Bush, the study opens up many questions, such as whether lithium levels in people decline with normal ageing, whether lithium is an essential element and what would be an optimal dietary intake. ‘Lithium orotate deserves to be tested in clinical trials for Alzheimer’s disease and mild-cognitive impairment,’ he adds.
Update: This article was amended on 12 August 2025 to add clarity to the discussion of lithium toxicity.
References
1. L Aron et al, Nature, 2025, DOI: 10.1038/s41586-025-09335-x
2. A Bush, Nature, 2025, DOI: 10.1038/d41586-025-02255-w















No comments yet