Pfizer–BioNTech’s will need to be one of many if we are to overcome the pandemic
Pfizer and BioNTech’s early peek at the effectiveness of their Covid-19 vaccine is encouraging, but there’s still a long way to go before a vaccine will be widely available.
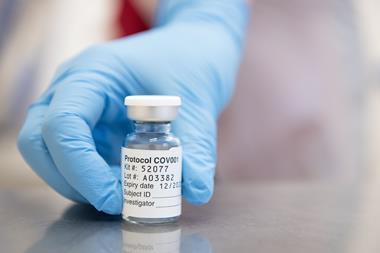
From this first glimpse at how things are going in trials, it seems that the vaccine will offer good levels of protection against the disease. Out of 43,500 people so far enrolled on the trial, over 90 have subsequently tested positive for Covid-19. Most of them had received a placebo, not the vaccine. The companies say this suggests the vaccine is at least 90% effective at preventing people from developing the disease.
As the trial progresses, with larger numbers of infections and more robust data analysis, we will get a better idea of how accurate this number is. However, efficacy is not the only reason for running these trials – safety is a huge factor. The US Food and Drug Administration has been clear that it needs to see a minimum of two months’ data after people are given their second dose of vaccine before it will consider applications for an Emergency Use Authorisation. Pfizer’s chief executive Albert Bourla projects that this will happen around the third week of November.
Even if all goes smoothly in the trial, there are still massive logistical hurdles to overcome. This vaccine is not going to be the answer for everyone, by any means. While the companies have been investing heavily in developing manufacturing capacity, this would be the first time such an RNA-based vaccine has been produced and distributed. Expecting everything to go without a hitch is probably wishful thinking. The fact that it needs to be stored at –70°C makes this especially difficult.
Maintaining cold chain transport for products kept at regular freezer or refrigerator temperatures is hard enough. But the need for specialised ultra-cold freezers and transport will severely limit where and how quickly the Pfizer–BioNTech vaccine can be deployed. Most likely it will, at least to begin with, be limited to large hospitals in developed countries with access to the necessary infrastructure.
Given that the people most desperately in need of vaccine protection are probably healthcare workers, this isn’t all that bad. But it does exaggerate the inequalities already present in global healthcare systems, almost automatically excluding remote areas and lower income countries even if their need is as great or greater.
Perhaps the most promising aspect of this preliminary view is the fillip it gives the other vaccines in development. It indicates that vaccines can work against the virus, even if the safety and efficacy profiles will vary. Given that several of the other vaccines in late stage trials should be simpler to manufacture and distribute, that can only be good news all round.















No comments yet