Around 30% of current cancer deaths in the US are caused by tobacco. According to the World Health Organization, tobacco is ‘the only legally available product that kills up to one half of its regular users when consumed as recommended’.
Although nicotine is addictive, it’s tar that kills. A meta-analysis of 35 clinical trials found no evidence of cardiovascular or other life-threatening adverse effects caused by nicotine intake, and nicotine did not increase cardiovascular risk, even in patients with established cardiovascular disease.1
This is perhaps why e-cigarettes have been proposed as a harm reduction option when it comes to smoking. If all smokers switched to e-cigarettes, and if current estimates about the risk of these products are accurate, cancer deaths would fall to only 1–2% of users.2 Sure, it’s not advisable to regularly inhale nicotine, and my nine-year-old will not find an e-cigarette under the Christmas tree, but what makes e-cigarettes so controversial when it comes to public health?
Matter for concern
One key aspect is whether e-cigarettes represent a gateway to regular smoking, and are making tobacco products more acceptable again. According to the US Centers for Disease Control and Prevention, around 2.4 million middle and high school students in the US were current users of e-cigarettes in 2014. Yet studies suggest that one in three smokers who switch to e-cigarettes reduce their consumption, and one in nine quit for good – numbers that will only rise as manufacturers increasingly make the experience mimic actual smoking. Whether e-cigarettes are a potent weapon for smoking cessation, or are simply a way for big tobacco to remain in business, depends on which studies you read.
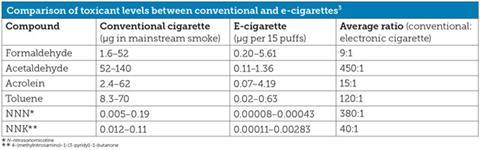
The chemical picture is even more complex. E-cigarette aerosol is not water vapour as is often claimed; it can also contain heavy metals and ultrafine particles, as well as carcinogens such as formaldehyde, acetaldehyde and acrolein (albeit at levels significantly lower than in cigarette smoke).3
The range of additives and flavours used by the devices also presents a challenge. Two years ago, one count came up with more than 3700 flavours available, including cheesecake and strawberry. Essentially, none of these flavourings has been tested to assess their risk to health; while many are food additives, just because they are safe when swallowed does not mean they are safe when inhaled chronically.
A good example is diacetyl, a compound found in 75% of e-cigarettes tested. The substance is quite well known – it is the butter flavour of popcorn. Although apparently safe when consumed, it is worth noting that inhalation of diacetyl has caused lung disease in workers producing the snack (known as ‘popcorn lung’).4 While it is not clear whether the amounts inhaled by e-cigarette consumption could cause such conditions, diacetyl shows that there can be surprises when inhaling food flavours.
Testing challenges
In a perfect world, we would embark on extensive trials of each and every one of these additives used. However, there are practical concerns that make this option difficult to achieve. Inhalation toxicity studies are very expensive, and rodent cancer tests even more so, costing around $1 million (£700,000) per substance in the current standard method. This would amount to $4 billion to test all the flavourings available. In addition, trials using rats are not always predictive of human physiology, and there is no generally accepted animal model of smoking-induced lung cancer.
It also takes four years to get the results from cancer studies and they notoriously err on the side of safety. For example, of more than 30 ingredients of coffee tested for carcinogenicity in rodents, more than 70% had a positive result. Does this mean we are regularly enjoying a brew of carcinogens? No – there is no such evidence. Some studies even show that coffee may reduce cancer risk.
In the short term, self-restricting the use of additives and using fast cell- and computer-based evaluations of safety will help clarify the safety of e-cigarettes. And in the medium term, controlled trials will be necessary. But if we wait for this evidence to emerge and prohibit or hinder the use of e-cigarettes, we would probably miss a tremendous opportunity to save lives on a large scale.
Thomas Hartung is Doerenkamp-Zbinden professor and chair for evidence-based toxicology at Johns Hopkins Bloomberg School of Public Health, US.
References
1 K Farsalinos and R Polosa, Ther. Adv. Drug Saf., 2014, 5, 67 (DOI: 10.1177/2042098614524430)
2 E-cigarettes: an evidence update, Public Health England, 2015
3 M Goniewicz et al, Tob. Control, 2014, 23, 133 (DOI: 10.1136/tobaccocontrol-2012-050859)
4 D Egilman, C Mailloux and C Valentin, Int. J. Occup. Environ. Health, 2007, 13, 85 (DOI: 10.1179/107735207800244893)











No comments yet