Eddie Heywood explains how having a range of drugs has helped a whole generation live with HIV – now their biggest concern is remembering to take them
I was diagnosed with HIV on 31 October 2011. I remember the date vividly as Halloween has always been my favourite day of the year.
Around the 2010s, significant advances were being made in HIV treatment. By that point we had access to Pep, or post-exposure prophylaxis, which was for when you knew there was a good chance you had been exposed to HIV – but this was a month-long treatment regimen that generally made you throw up. Studies for Prep, or pre-exposure prophylaxis – which you can now take proactively to minimise the risk of contracting HIV - were only really kicking off when I got infected.
At that time, I was getting tested for HIV every three months at a sexual health clinic and did not expect this visit to be any different – a rapid fingerprick test and then 15 minutes spent waiting for the result. But on this occasion the clinician came back and said the test had come back as reactive, potentially indicating HIV infection.
I was dating someone who worked in sexual health care in the US, specifically within HIV outreach, so I was very well informed about what the next steps would be. But it didn’t make it any easier – those two weeks waiting for my full blood test results were harrowing.
A fortnight later I went back into the clinic with a friend and received my life-changing diagnosis. Although an HIV diagnosis is no longer a death sentence, you never know how you’re going to react to the treatment and even if you react well, it’s still a lifetime of taking medication – there’s no going back, there’s no cure.
Thankfully, because I had been getting tested regularly, they caught it early while I still had quite a healthy immune system with no signs of infection. The difficult thing with HIV is it progresses at a different rate in different people. It can take two years to absolutely destroy your body or it can take 20 years, but because I was dating someone who was HIV-negative, I elected to go on medication as soon as possible.
Living in London I was very lucky that there was a lot of provision for HIV care – the doctors at the clinic gave me a lot of agency, self-determination and help in deciding the approach I wanted to take with my treatment. Outside of the big cities it can be a lot more challenging – GPs may be less up to date with testing and retain certain prejudices.
It might have only been three pills a day but there were also the drugs you had to take for the side effects
I have a lot of other complicated health issues so the doctor had to test for different allergies to the potential medications. Fortunately, compared to the 1980s when there was pretty much one horrible pill that you had to take multiple times a day, there were a vast array of options.
I was not able to take the first- or second-line medication because of mental health issues – a lot of HIV drugs can cause suicidal ideation – so I was put on atazanavir, ritonavir and Truvada (emtricitabine and tenofovir disoproxil); three pills taken once a day. For the first month to six weeks of taking antiretrovirals (ARVs) many people have headaches, nausea, weight fluctuations and sometimes jaundice.
Luckily my side effects were not so bad that I had to take additional pills to treat them – that was always a big thing with the earlier drugs: it might have only been three pills a day but there were also the drugs you had to take for the side effects.
As a result, adherence is a big issue with HIV treatment. About four months in I became really fed up of taking them – it was a daily reminder of this horrible thing inside my body – so I decided not to. I then really regretted it and worried about the effect it might have on my partner and that gave me the necessary shock to continue.
Now there’s a huge range of different options and usually people can find something that works well for them
I do still have wobbles though. During the Covid-19 pandemic my adherence went down to about 85%. That’s when I had to engage with an adherence specialist who reminded me of the additional flexibility with modern treatments that are well tolerated; even if you only have 12 hours between doses it’s still better than not taking it at all.
Around 2017, I switched to Evotaz (combination of atazanavir and cobicistat) which was one pill a day, so nice and easy. I changed medication again just before the pandemic – as I had plans to move to Canada and the drug I was on were not always available there. So that’s when I went on to Delstrigo which is a combination of three medications (doravirine, lamivudine and tenofovir disoproxil) in one pill .
Even in the last 10 years, I’ve witnessed a dramatic shift in the medication that’s available to treat HIV. Now there’s a huge range of different options and usually people can find something that works well for them. There’s also been changes in terms of reducing the risk of HIV – first with Pep and now with Prep – and it’s now clinically proven that HIV-positive people on effective medication with undetectable levels of the virus cannot pass it on sexually: undetectable = untransmissible (U = U).
The availability of these new drugs, along with communications outreach and the U = U campaign, has helped lift some of the stigma associated with HIV, because it’s no longer a death sentence – this is the first time we have a generation of gay men who are growing up with HIV and their life expectancy is just the same as people that don’t have it. Most people I know that have been diagnosed are coping well – their biggest worry is remembering to take their medication.
As told to Julia Robinson

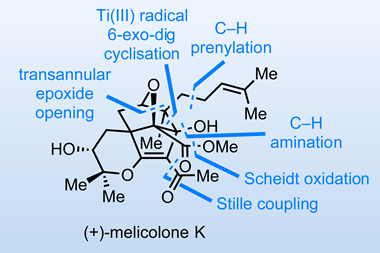
How HIV drugs have changed over the decades
From one big pill that only prolonged lives a few months, through the 20 pills a day years to modern combination therapies, treating HIV is a science success story
- 1
 Currently
reading
Currently
reading
How advances in antiretrovirals have impacted my life with HIV

















No comments yet