Although TB was close to being eradicated in the developed world, it is a major problem in developing countries. With drug-resistant strains on the increase, Clare Sansom outlines the latest in the fight against this killer disease
From a historical viewpoint, what is the world’s most deadly infectious disease? Tuberculosis (TB) must be one of the strongest contenders. The disease that the seventeenth-century writer John Bunyan described as ‘the captain of all the men of death’ is still rightly feared today. Despite some recent progress, the latest figures released by the World Health Organisation (WHO) show that there were an estimated 8.8 million cases of active tuberculosis and 1.4 million deaths from the disease in 2010.
But the current WHO guidelines for managing tuberculosis describe it as ‘treatable and curable’, so why is it still such a worldwide problem? Control of any infectious disease can be divided into three areas: prevention (including vaccination), diagnosis and treatment, and progress in each of these areas has been painfully slow for most of the 130 years since TB’s cause was discovered. The only widely used vaccine against TB has been around for 90 years, and no new drugs against the disease have entered the clinic for over 40. Cases are too often misdiagnosed or missed altogether.

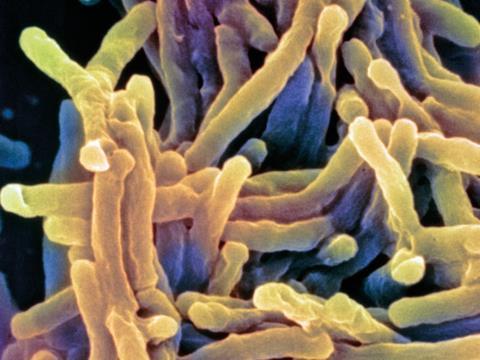
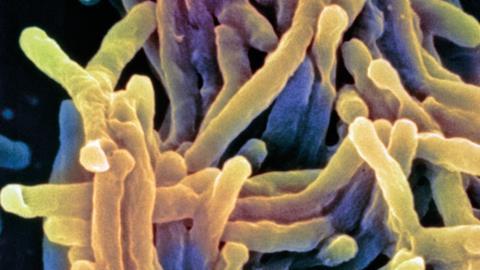
The eponymous bacterium that causes TB, Mycobacterium tuberculosis, was discovered by Robert Koch, who also formulated the postulates that bear his name for establishing the cause of an infectious disease. It is an unusual beast, much slower to grow than most bacteria, and with a characteristic thick coat principally made of mycolic acids. It infects the lungs of its human host, where it is taken up by macrophages – the cells that remove debris and pathogens by engulfing and digesting them. Unfortunately, TB bacilli can live within them for many years without causing the active disease and it has been estimated that about a third of the world’s population carry this ‘latent’ form of TB.
Complex therapy
Tuberculosis has historically been associated, under its former name of consumption, with a number of notable literary and intellectual figures. Keats and Chopin suffered from the disease, as did George Orwell, who used some of the royalties from Nineteen Eighty-Four to import streptomycin – the first drug to prove at all effective against tuberculosis – from the US. Nowadays, however, ‘the burden of TB is carried by the most vulnerable’ according to Mario Raviglione, director of the Stop TB Department at the WHO. This refers to the world’s poorest people, who live in crowded, unsanitary conditions, and often suffer from other conditions that increase the odds of latent disease becoming activated. HIV is the most important of these: the ‘deadly synergy’ between AIDS and tuberculosis has often been described in the literature. Latent TB is over twenty times more likely to become active in people who are HIV positive than in those who are not.
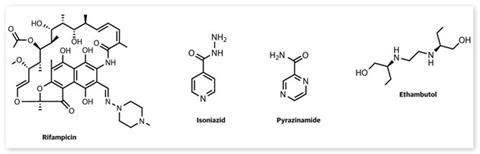
The current treatment regimen for drug-sensitive tuberculosis is long and complex, involving four drugs from different chemical classes. Patients are treated with isoniazid, rifampicin, pyrazinamide and ethambutol for two months, then just isoniazid and rifampicin for a further four. Understandably, many people find this regimen difficult to follow, especially as each of these drugs has side effects: isoniazid can cause neuropathy, which is exacerbated in people with HIV, and rifampicin can be toxic to the liver. The WHO therefore recommends the DOTS (directly observed therapy, short course) strategy where a healthcare worker directly observes patients taking their medication. This has now been widely, although not universally, adopted, but it is hardest to maintain in the poorer countries and difficult conditions where tuberculosis flourishes most easily.
The complex nature of the ‘standard’ tuberculosis therapy is only the tip of the iceberg of problems with treating TB. Multi-drug resistant (MDR) tuberculosis, in which the bacteria are resistant to at least isoniazid and rifampicin, has now been identified in almost every country. Patients diagnosed with this form of the disease have to endure two-year courses of treatment with toxic second-line drugs; the cost of treating a single patient with MDR-TB in the UK has been estimated at £50,000–£100,000. Extensively drug resistant tuberculosis, which responds to even fewer drugs, has also been widely reported, as has a form of totally drug resistant TB in countries as diverse as Italy, Iran and India.
Politics and money
The political will to tackle tuberculosis, along with other infectious diseases of the poor, may have reached an all-time low in the years before the AIDS epidemic brought infection back into the centre of public consciousness. Since then, and more particularly since the turn of the millennium, TB has moved closer to centre stage. It is the only ‘other disease’ to be mentioned explicitly in the targets set for the UN’s Millennium Development Goal 6 (to ‘combat HIV/AIDS, malaria and other diseases’). During the last ten years, governments, companies and private philanthropists have channelled huge sums by historical standards into tuberculosis prevention and care through the Global Fund to Fight AIDS, Malaria and Tuberculosis.
This fund, however, did not escape the effects of the global financial crisis: the eleventh and most recent funding round had to be cancelled in November 2011 due to a shortfall in donations, most markedly from governments. This threatened to derail much excellent work until the cause was taken up by, among others, the All-Party Parliamentary Group on Global Tuberculosis, a group of UK politicians with an interest in TB. ‘Even in these austere times, we managed to persuade the UK government to double its contributions to this fund, and others are doing the same, so with any luck it should soon be back on track’, says Simon Logan, policy adviser to this group.
The Global Fund has no remit to fund the discovery and development of diagnostics, drugs or vaccines. Much of the recent progress that has been made in these areas – and since the turn of the millennium this has been considerable – has been driven by the academic and small biotech sectors, and by developments in genomics. The tuberculosis genome was published in 1998, only three years after that of the first free-living organism. It is large for a bacterial genome, with four million base pairs and 3959 protein-coding genes. About 250 of these are involved in the metabolism of fatty acids, including those comprising its complex cell wall.
Diagnosis and drugs
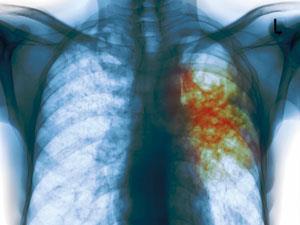
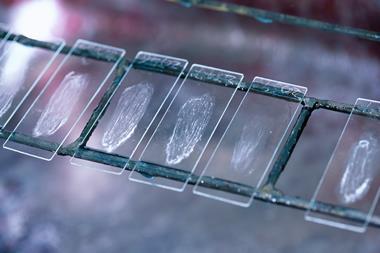
But all the money in the world will not produce a cure for tuberculosis if interdisciplinary science fails to deliver. For tuberculosis (or any disease) to be treated effectively, it must first be correctly diagnosed. Ruth McNerney from the London School of Hygiene and Tropical Medicine, UK, explains the extent of the problem: ‘We still don’t know exactly how much TB there is in the world. We estimate that about a third of people don’t get diagnosed, so they’re not treated, and, of course, they remain infectious.’ Until very recently, the main method for diagnosis involved a chest X-ray followed by a difficult culture of the slow-growing bacterium from a sample of blood or sputum.
The first molecular system for the diagnosis of TB, Cepheid’s GeneXpert, was endorsed by the WHO at the end of 2010. This simple-to-use PCR-based platform can return a diagnosis of TB in no more than an hour. Its only real disadvantage is its high cost; even at the latest subsidised rate of $10 per test, it is unaffordable in many developing countries. ‘Technical improvements and competition from rival companies will bring the price down further, but it will probably always remain out of reach of some who need it,’ says McNerney. She is also concerned that diagnosis is still crude: ‘There is an urgent need for more biomarkers. We need to be able to look at a whole panel of antibodies and antigens at once, to distinguish between latent and active TB and to tell how drug resistant a sample is,’ she adds.
After diagnosis comes treatment. Drug discovery programmes typically focus on a specific unmet medical need, and tuberculosis can offer many of these. It is clear that a wider range of drugs is needed, particularly to combat resistant strains. Further priorities are shorter, simpler treatment regimens for TB that is not yet resistant to drugs, which would be less toxic and easier for patients to follow, and more appropriate treatments for co-infections with HIV. Finally, there are no drugs at all for latent TB infection: such a drug, which could prevent both symptomatic illness and the spread of the disease, could be almost as effective in controlling it as a vaccine. In all cases, cost will always be a serious concern. ‘We need to develop new drugs, but we also want them to be on the market and affordable in countries with a high TB burden,’ says Logan.
After the publication of the first bacterial genome sequences, much early-stage drug discovery was target-based. Many researchers used bioinformatics and structural biology to select and elucidate the details of the proteins considered both essential for bacterial metabolism and relatively easy to be inhibited by small-molecule drugs. Recently, however, the use of phenotype-based assays to select candidate molecules without prior knowledge of their mechanism of action has made something of a comeback. ‘The target-based approach has generally failed to deliver [in drug development for TB]’ says Geoff Coxon, a medicinal chemist from the University of Strathclyde, Scotland and Tuberculosis Drug Discovery UK.

Many scientists advocate a two-pronged approach incorporating both target-based and phenotype-based methods, Sanjib Bhakta from Birkbeck, University of London UK, among them. His group has developed a fast phenotypic screen – SPOTi – that can evaluate the potential anti-tubercular properties of as many as 2,000 molecules in six months. They have also published structural studies of the Mur ligase family of enzymes that are essential for the formation of the mycobacterial cell wall. ‘We are collaborating with medicinal chemists in University College, London, to develop hit molecules from both these screens into leads, and GSK is already interested in taking really promising molecules into clinical trials,’ Bhakta says.
Showing promise
The later-stage drug development pipeline is finally beginning to fill with promising candidate drugs. Two molecules with different novel targets – bedaquiline, developed by Janssen (now part of Johnson & Johnson) and Otsuka’s delamanid – are now entering Phase III clinical trials.
Bedaquiline, discovered through a phenotypic screen and believed to be active against both drug-sensitive and drug-resistant TB, has an unexpected target: mycobacterial ATPase. ‘Nobody would have ever picked bacterial ATPase as an interesting target for anti-TB drugs, because of its perceived similarity with human mitochondrial ATPase,’ says Koen Andries, a distinguished research fellow at Janssen. ‘Despite this similarity, there are a few key amino acid differences in the enzyme active site, and these are enough to lead to drug specificity. This is a lesson to drug developers: a [bacterial] protein should not be excluded as a drug target because it has a human homologue.’ Janssen has taken the molecule through Phase II clinical trials against MDR-TB, with trials against the drug sensitive disease being undertaken by the non-profit Global Alliance for TB Drug Development.
Otsuka’s molecule, an imidazooxazole, is also showing particular promise against drug resistant strains of tuberculosis. It blocks the synthesis of two mycolic acids that are necessary in mycobacterial metabolism. ‘Phase II trials have shown that adding delamanid to the standard treatment for MDR-TB can increase the response rate significantly,’ says Larry Geiter, vice president for global clinical development at Otsuka.
A Phase III trial of delamanid in MDR-TB has just started, and the company filed a new drug application to the European Medicines Agency for this drug in MDR tuberculosis in December 2011. In July 2012, Johnson & Johnson filed an new drug application for bedaquiline with the US Food and Drug Adminstration against the same condition. If or when either application leads to a full registration, that drug is likely to be the first novel anti-tubercular to enter the clinic in almost half a century. There is still a long way to go, however. ‘Late stage clinical trials for tuberculosis are long and complex, and require patients to be recruited internationally; it is particularly difficult to find enough patients with definitively diagnosed drug-resistant TB to fit a trial protocol,’ says Patrick Phillips, a senior statistician at the MRC Clinical Trials Unit in London. ‘They will therefore often be run as collaborations, sometimes involving both the public and private sectors.’
These are exciting times for tuberculosis research and drug development, and there are grounds for optimism that the long wait for new medicines will soon be over. Fourteen years after the publication of the TB genome, it is possible to imagine a time when the cocktail of drugs to treat an individual tuberculosis patient might be tailor-made using knowledge of the genome of the bacteria infecting them. This ‘personalised medicine’ for tuberculosis patients should become technically possible before very long, but it will remain expensive: ‘Investment in technology transfer will be needed to make sure that new diagnostics and drugs reach those who need them most, the most vulnerable,’ says Raviglione.










No comments yet