Chemical model reveals how alcoholism drug disulfiram joins copper to kill cancer cells with oxidation overload
When copper meets alcoholism drug disulfiram they form a deadly union that dodges cancer cells’ defence mechanisms and kills them through oxidative stress. Exactly how the drug works has now been unravelled by a team of scientists from China.
Disulfiram has been used for almost 70 years as an anti-alcoholism drug. It produces acute ethanol sensitivity, including immediate and enhanced hangover effects, by stopping the body from breaking down acetaldehyde. But two years ago, scientists found its copper complex also has anticancer activity. How exactly the drug does this, however, remained unclear.
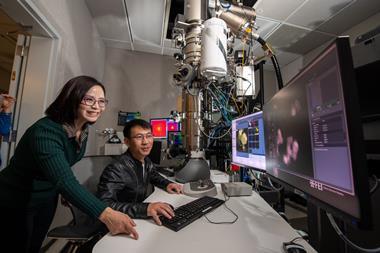
A team around Wei Deng from the Shanghai Institute of Technology, Yu Wang from the Chinese Academy of Sciences and ShanghaiTech University’s Bolin Lin has designed a simplified chemical model to understand disulfiram’s cancer-killing ability.
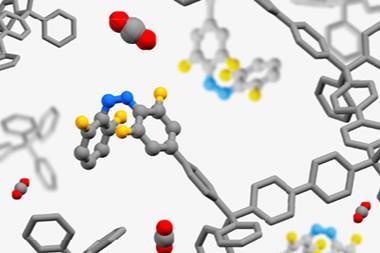
They looked at what happens to copper(II)diethyldithiocarbamate (DTC), a disulfiram metabolite, when faced with a zinc(II) complex and two thiols, ethanethiol and dithiothreitol. In living systems, thiols and nicotinamide adenine dinucleotide (NADH) protect zinc thiolates from oxidation. This is essential for the cell’s survival, since these zinc fingers are part of many vital proteins.
As it turns out, copper DTC came out winner in competition experiments. ‘DTC displays a unique redox-tuning ability that enables copper to resist the reduction by thiols and NADH while retaining its ability to oxidise zinc thiolates,’ Lin explains.
Once oxidised, zinc fingers lose their biological function and the cell dies – at least that’s the theory. ‘The model studies do give us clear ideas about the fundamental chemical reactivities and selectivities,’ says Lin. ‘Living systems are, of course, much more complicated.’
Cancer researcher Michael Carducci from Johns Hopkins School of Medicine, US, has reservations. He trialled a similar copper chelator for treating prostate cancer. ‘[It] showed no clinical benefit. We showed that it reduces copper levels, but did not have any clinical output.’
Lin’s team will now extend its studies to biological systems. One important question is whether disulfiram can form the active copper complex where it’s needed – in tumours rather than in healthy cells. The team’s hypothesis is that tumours accumulate more copper than non-cancerous tissue.
Wolfgang Maret, a metalloenzyme researcher at King’s College London, UK, thinks disulfiram and its copper complex might have different biological targets entirely. ‘In disulfiram, you have the disulfide as the oxidant. Now in [copper DTC], you have to have the copper as the oxidant, so pharmacologically, that’s quite interesting – if it works in animal experiments.’
‘I wouldn’t hold out hope for specifically disulfiram [to become a cancer drug],’ says Carducci. ‘But maybe their work is going to allow for development of molecules that can affect these pathways and be potentially more specific to cancer cells.’
References
L Xu et al, Angew. Chem. Int. Ed., 2018, DOI: 10.1002/anie.201814519











No comments yet