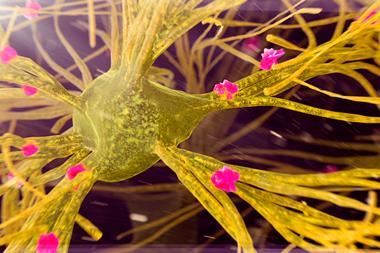
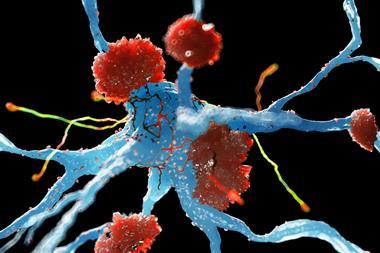
An excess of fragments of amyloid precursor protein (APP), called APP-CTFs, can trigger a mechanism that occurs at the early stages of Alzheimer’s disease. The researchers say understanding the role of APP-CTFs could open avenues for early intervention therapies that could stop or even prevent Alzheimer’s disease.
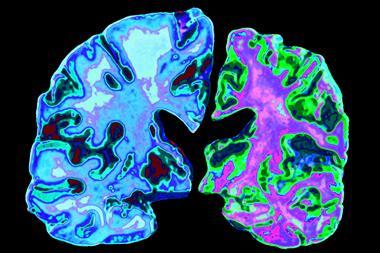
For the past two decades, Alzheimer’s research has focused on events that occur much later on in the disease: amyloid-β plaques in the brain and, more recently, the presence of tau and microglia. ‘To prevent Alzheimer’s disease we need to understand what happens in the brain before the typical hallmarks appear: this can be up to 10 years before a clinical diagnosis is set,’ says senior author Wim Annaert at KU Leuven and VIB-Center for Brain and Disease Research in Belgium. Previous studies have shown that abnormal endosomes and lysosomes in neurons occur long before amyloid plaques appear and are common in both forms of Alzheimer’s disease, familial and sporadic. And although toxic APP-CTF has been linked to this dysfunction, nobody has been able to really join the dots. Until now.
Annaert and his colleagues used Crispr–Cas9 gene editing to deactivate or ‘knock out’ PSEN genes in embryonic fibroblast mouse cells and neurons. PSEN genes provide instructions to make presenilin proteins, crucial for the function of γ-secretase which cleaves APP into amyloid-β peptides. With super-resolution imaging they were able to show that inactivating γ-secretase resulted in the build-up of APP-CTFs, which greatly reduced calcium ion uptake in lysosomes. This could lead to the collapse of endolysosomes’ ability to effectively break down and recycle substances and, ultimately, cell death. The team removed APP-CTFs by knocking out the APP gene which restored normal endosomal functions. ‘This allowed us to conclude that γ-secretase is required to keep the balance of APP-CTFs in check and prevent their toxic overproduction,’ says Annaert.
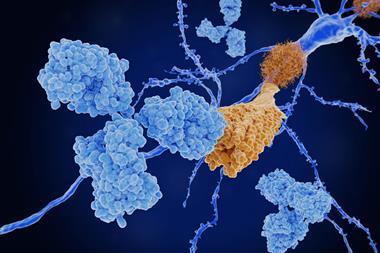
Therapeutic approaches have tended to lean towards the removal of amyloid-β plaques by inhibiting the activities of γ-secretase and β-secretase – which together are key to the production of amyloid-β – or neutralising it once formed with antibodies. However, most of these clinical trials have failed, many with toxic side effects. ‘[Amyloid plaques] is a relatively late event and any effective drug will only delay disease progression,’ says Annaert. The researchers in this study say the toxicity of APP-CTFs may have contributed to the failure of clinical trials.
Studies have shown that amyloid-β and APP-CTF can accumulate in tandem with one another, but researchers have largely overlooked this. ‘This knowledge can lead to a smarter drug design that both prevents the accumulation of toxic amyloid-β peptides and APP-CTFs,’ Annaert adds. These could include γ-secretase modulators that stabilise – rather than turn off – the activity of γ-secretase, making shorter, non-toxic amyloids, and may prevent APP-CTF accumulation.
Gunnar Gouras, a neurologist at Lund University who was not involved in the study, believes APP-CTF could be a possible drug target in the future, but thinks it’s too early to say how effective it will be against Alzheimer’s disease. ‘Presenilin inhibition is not a common feature in Alzheimer’s disease, except for in familial forms of Alzheimer’s with presenilin mutations,’ he says. Gouras suggests the next step should be to investigate the link between presenilin mutations and the disease in mouse models. ‘But increasing evidence is supporting an important role of APP-CTF in the disease,’ Gouras highlights.
References
M Bretou et al, Dev. Cell, 2024, 59, 1–22 (DOI: 10.1016/j.devcel.2024.0f3.030)







No comments yet