Alzheimer’s disease can be transmitted between people in rare circumstances as a result of medical procedures. This discovery comes following an investigation of unusually young Alzheimer’s patients in the UK who had all received growth hormones as children.
The hormones came from the pituitary glands of deceased individuals, a procedure banned in 1985 after it was linked to the transmission of misfolded proteins – prions – that cause Creutzfeldt–Jakob disease (CJD).
Between 1959 and 1985, at least 1848 patients were treated with human growth hormone from human pituitary glands, resulting in over 200 cases of CJD, with 80 in the UK alone. Now it seems the procedure also put people at risk of contracting Alzheimer’s disease. The UK research group behind the work has also warned that more growth hormone was likely to be contaminated with amyloid beta than with CJD prions and have a longer incubation period to Alzheimer’s than CJD.
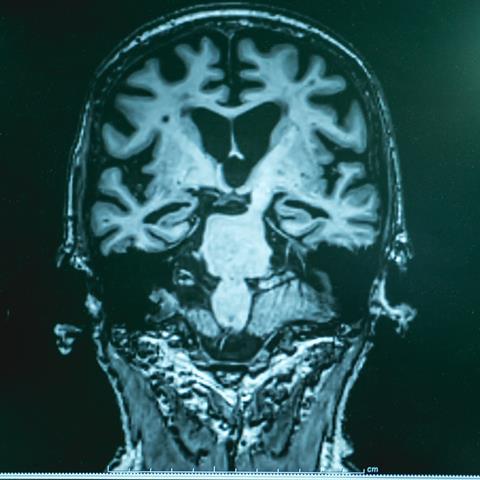
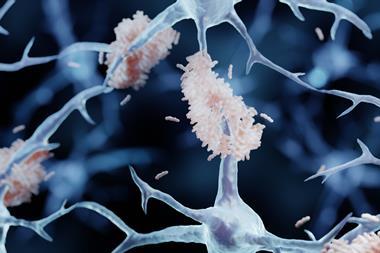
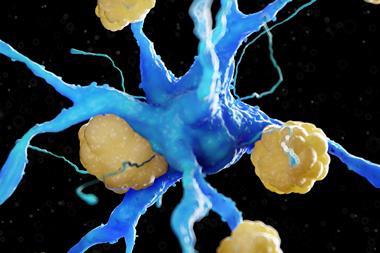
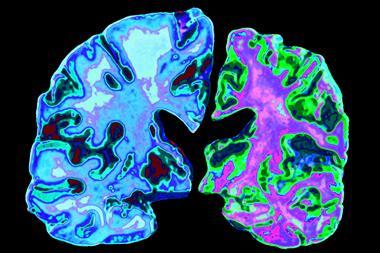
The first hints that Alzheimer’s disease is transmissible in very specific circumstances emerged when neurologists at University College London (UCL) examined the brains of eight people with medically acquired CJD. They unexpectedly saw signs of Alzheimer’s disease in the form of clumps of amyloid beta protein, or amyloid plaques, in grey matter – a telltale hallmark of this progressive brain disease.
The UCL researchers’ suspicions were backed by the fact that tissue from human Alzheimer’s brains was known to be able to seed amyloid beta plaques in the brains of mice. In 2018, the team obtained stored batches of growth hormone extracted from pituitary glands and showed that they could seed plaques of amyloid beta in mice.
The eight patients who developed cognitive impairment had been referred to the National Prion Clinic in London and five of them went on to show symptoms that matched Alzheimer’s disease. An autopsy of one of two patients who died during the course of the study revealed that they had signs of Alzheimer’s disease.

The five who displayed Alzheimer’s disease ‘were a little bit different from what you might call classical Alzheimer’s’, says John Collinge, the neurologist at UCL who led the study. He adds that this wasn’t a surprise as contaminated growth hormones are a very different way of developing the disease.
‘It is a small number of subjects, but it is striking that their amyloid pathology looks like early-stage Alzheimer’s yet you don’t see a lot of tau pathology,’ says Paul Murphy, an Alzheimer’s researcher at the University of Kentucky. Tau tangles are thought to follow amyloid plaques and kill a lot of neurons, he explains, which then causes cognition problems.
The vast majority of Alzheimer’s disease happens out of the blue, with patients showing symptoms after age 65. A second form can occur earlier in life as a result of certain genetic mutations. This new study points to a third, acquired form of Alzheimer’s.
‘You can have these very rare cases, just like in CJD, where people are accidentally exposed to these transmissible seeds as a result of a medical procedure,’ says Collinge. ‘The majority of this relates to medical procedures that are no longer used.’
For CJD, this includes the grafting of brain membrane to repair defects during neurosurgery and corneal transplants, as well as through contaminated surgical instruments. Most CJD happens sporadically or through inherited mutations, with around 1% estimated to be acquired.
Alzheimer’s disease researcher Bart De Stroop at UCL, who was not involved in the new study, says increased vigilance is warranted, especially around procedures in early life that involve human fluids or tissues. He suggests closely following what happens to patient groups that have procedures such as blood transfusion or organ transplantation. ‘That is what is needed most to understand how big an issue this is,’ he notes. ‘At this moment, it looks like a very rare phenomenon.’
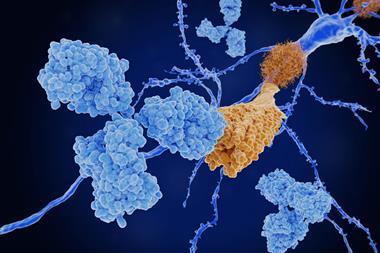
Collinge also warns that their research suggests encouraging results from monoclonal antibody therapies for Alzheimer’s disease could be premature. ‘We know that in prion disease, if you develop a drug which binds to the majority of components of a main strain [of prion] that is propagating in the brain, you can get the rapid development of resistance from minor species that are present,’ he says.
Murphy calls this idea ‘fascinating’, but says that it appears that there is one type of amyloid beta protein that is particularly harmful in Alzheimer’s disease and any therapy that can get rid of this early enough should make a difference to patients.
References
G Banerjee et al, Nat. Med., 2024, (DOI: 10.1038/s41591-023-02729-2)