Dual-organ simulation uncovers possible toxicity mechanisms that result in liver injury
A microfluidic device that recreates interactions between the gastrointestinal (GI) tract and the liver to give a more realistic assessment of nanoparticle toxicity has detected liver tissue injury at lower nanoparticle concentrations than expected following experiments with liver tissue only.
Many studies look at the beneficial medical effects of nanoparticles, however, Mandy Esch explains that her work in Michael Shuler’s lab at Cornell University is checking for adverse effects.
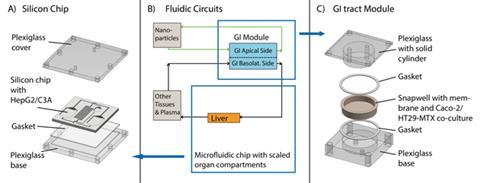
Esch has made microfluidic silicon chips with separate chambers containing different tissue analogs in the form of cell cultures. This body-on-a-chip device is a miniaturised model of a section of the human body, scaled down by 400,000. Two fluidic circuits connect the basolateral side of the GI tract module with the silicon chip and the liver container.
HepG2/C3A cells were used to represent the liver, with the intestinal cell co-culture consisting of enterocytes (Caco-2) and mucin-producing (HT29-MTX) cells. Carboxylated polystyrene nanoparticles were fluorescently labelled so their movement between the chambers could be tracked. Levels of aspartate transaminase, a cytosolic enzyme released into the culture medium upon cell death, were measured to give an indication of liver damage.
The study saw that single nanoparticles and smaller nanoparticle aggregates were able to cross the GI barrier and reach the liver cells. The increased zeta potentials of these nanoparticles suggest that crossing the barrier may raise their toxic potential. However, larger nanoparticles, which interact with cell membranes and aggregate into clusters, were stopped much more effectively by the GI tract barrier.
The gastrointestinal tract is an important barrier preventing ingested substances crossing into systemic circulation. Initial results indicate that soluble mediators released upon low-level injury to liver cells may enhance the initial injury by damaging the cells which form the GI tract. These adverse effects were not seen in conventional single-organ tests.
Hyun Jung Kim, a bioengineer at Harvard University, US, understands the importance of microengineered devices that can recreate specialised multicellular architecture, to successfully evaluate nanoparticle absorption and hepatoxicity. He believes that this work by Esch and the team ‘highlights how microfluidic organ-on-a-chip technology can provide new in vitro tools for mechanistic studies of drug and environmental particle absorption, metabolism and toxicity’.
Future experiments using 3D constructs of tissues will make the simulations more realistic and allow for more authentic physiological behaviour to be observed.
References
This paper is free to access until 12 August 2014. Download it here:
M Esch et al, Lab on a Chip, 2014, DOI: 10.1039/c4lc00371c









No comments yet