Catching the citizen science bug
Involving the public in research tackling superbugs
As part of the process of preparing for an upcoming surgery, my local hospital not only sent me for some blood tests and a routine electrocardiogram, but also for some swabs. The aim was to determine whether I was carrying some of the best-known antibiotic resistant infections, prior to my admission.
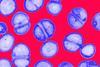
This caution is absolutely warranted. Antimicrobial resistance (AMR) is one of the leading causes of death and health care settings such as hospitals carry an increased risk of infection. Where patients recover from AMR infection, they commonly experience longer hospital stays, more complex interventions and recurrent infection.
Breaking the mould
Tackling AMR is a difficult challenge, particularly as our use/misuse of antibiotics is partly to blame for the emergence of drug resistance in some bacterial strains. Like most ‘wicked problems’ new approaches are required to solve not only the scientific questions raised but importantly to increase awareness of the need for behavioural change in prescribing or taking antimicrobials. In recent years, a number of citizen science projects have emerged, each aiming to connect members of the public to research relating to AMR.
