Regulating the line between a vital service and grey-market profiteering is a mess
‘Compounding pharmacies’ are a bit of an alternate universe in drug distribution. That’s quite a change from the way things were a hundred years ago, when compounding pharmacies were basically the only kind of pharmacy there was, but modern manufacturing practices changed all that. In a compounding pharmacy, individual ingredients are combined on site: the active drug or drugs, along with the liquid or solid formulation mixture that it’s given in. These are often done for individual patients – for example a person with a severe allergy to some ingredient in the standard commercial formulation of a medicine that they need, or a young child who is unable to swallow a large tablet and needs a liquid dose instead.

These are certainly legitimate medical needs, and compounding pharmacies can be the only way to meet them. But their operation can end up in some grey areas. For example, what if they are producing an alternate formulation not because of some medical reason, but just to lower the price of the final product (‘economic compounding’, as it’s known)? Or if they’re diverting the active ingredient in some other form of a popular drug to fill demand? That’s happening right now with the GLP-1 agonist diabetes and weight loss drugs like semaglutide, with very strong economic temptations to fill the rapidly increasing demand through any means available. The laws in the US and Europe do not clearly address some of these situations (and the laws across Europe are something of a patchwork in this area to start with).
On top of this, compounding is not without risks, particularly with injected drugs. The relatively light regulation in this area can lead to tragedies, as happened with the New England Compounding Center in 2012. This company (which was not a very long drive from where I live in Massachusetts) was preparing epidural steroid injection formulations for use in spinal cord patients, but they were doing so in a reckless way that led to hundreds of people suffering fungal meningitis and other infections. Dozens of patients died as a result, and the blame was completely on the compounding centre, which was sending out injection vials contaminated with black mould. (It was also in violation of the law, which allowed it to operate for the benefit of individual patients, not as a bulk supply facility). And in 2015, several patients at a hospital in Florence, Italy, developed eye infections from a contaminated compounded version of an antibody injection.
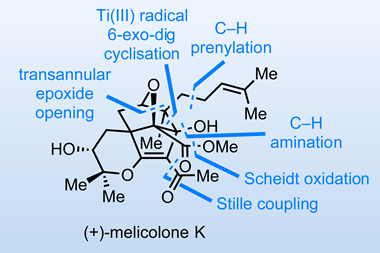
Other problems can occur when a compounding pharmacy changes the supply chain to provide a drug. Different salt forms are only the beginning of this (and those can by themselves be enough the change the properties of a drug once formulated). There are reports of compounding pharmacies sourcing ingredients through various ‘grey market’ channels of varying quality. Some of these are legitimate drug lots resold by middlemen (through transactions of variable legality!) but others are manufactured by facilities that aren’t approved as suppliers in the pharmacies’ own countries. To be fair, the pharmacies themselves may not even be aware of this latter problem by the time the ingredients become available to them, but that doesn’t make the problem go away.
There have been a number of attempted legislative fixes for these problems over the years (both in Europe and the US), but it’s a difficult area to regulate. Compounding, by its very nature, is going to be a heterogeneous business, dealing with a wide variety of drugs and an even wider variety of patients. And since it will always involve remixing things to order, you’re dealing with what are essentially tiny drug manufacturing facilities in each pharmacy. Inspecting these (and even keeping track of them in general) is just as difficult and messy as it sounds: the New England Compounding disaster occurred partly because the US Food and Drug Administration (FDA) thought it was the State of Massachusetts’ job to regulate, while the state thought it was the FDA’s! Add in the different motivations for compounding in the first place on the medical-economics spectrum, and you have a real regulatory nightmare. Which is why after all this time, the problem is still with us. Perhaps a system will emerge with fewer compounding pharmacies overall, with more stringent inspections, serving people through internet connections and mail order? That might be rational, but it won’t be easy to implement – a phrase that applies all too often in this business!














No comments yet