Novo Nordisk and Eli Lilly have struggled to meet huge demand for new hormone mimic obesity treatments
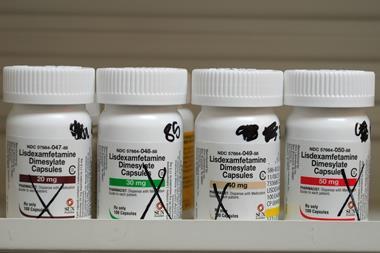
Soaring demand for new hormone-mimicking diabetes and anti-obesity drugs, coupled with difficulties in scaling up supplies, have led to severe shortages. Both Novo Nordisk and Eli Lilly have taken legal action to try and limit efforts of compounding pharmacies and wellness spas making copycat versions of their drugs in the US, while outright counterfeits are surfacing in several markets.
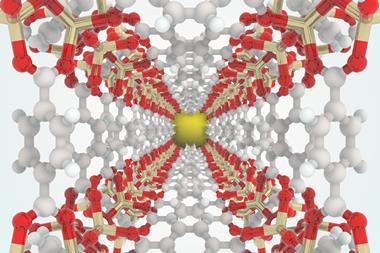
Glucagon-like peptide 1 (GLP-1)-mimics target brain receptors involved in appetite control, among others, and have been approved to treat diabetes for several years. However, when patients reported weight loss on these drugs, companies began to consider them as a treatment for obesity.

Novo’s semaglutide was approved in 2017 for diabetes (sold as Ozempic). After its approval to treat obesity (as Wegovy) in the US in 2021 and Europe in 2022, the company underestimated the growth in demand. Contamination problems at Novo’s US site making semaglutide (for tablet-based diabetes treatment Rybelsus rather than Ozempic and Wegovy) possibly added to supply constraints. ‘The shortage is immense,’ says Fatima Cody Stanford, an obesity medicine physician at Harvard Medical School in Boston, US.
Meanwhile, Lilly has also struggled to meet demand for its GLP-1 analogue, Mounjaro (tirzepatide), which was approved for diabetes in the US, Canada and Europe in 2022. It had been used off-label for obesity since its introduction, but its formal approval for treating obesity came in early November in the US (where it will be marketed as Zepbound) and the UK, and it has been recommended for approval by a European Medicines Agency (EMA) advisory committee.
Some compounding pharmacies are not quite following the letter of the law
Demand has been further stoked by celebrity attention. ‘Wegovy has been used widely for weight loss and has become a sort of viral hit, with [actors] and public figures showing its effects on social media,’ says David Margraf, pharmacologist and expert in drug supply at University of Minnesota, US.
Ozempic and Wegovy were placed on the drug shortages list of the US Food and Drug Administration (FDA) in May. And those shortages are impacting treatment. Stanford says the three starter-doses of Wegovy have been unavailable since the summer, so she has been unable to start new patients on the drug. On 10 November, Novo announced plans to invest DKK42 billion (£5 billion) to upgrade its manufacturing facilities to support GLP-1 products as well as other treatments for chronic diseases.
Counterfeits and compounding
The high prices of these drugs, coupled with shortages, have created a significant opportunity for counterfeiters. The EMA warned in October about falsified Ozempic injector pens identified at wholesalers in the EU and the UK. There were reports of people hospitalised in Austria after using counterfeit injectors possibly containing insulin, rather than semaglutide. In June, Novo Nordisk warned about a counterfeit Ozempic injector bought in a US pharmacy and containing insulin. Hundreds of fake Ozempic pens were reportedly seized in the UK this year. Dubious online ‘pharmacies’ offering direct sales of products claiming to include semaglutide have also proliferated, along with social media scams.
‘There are some drugs that you can make easily enough, but this is a more complicated molecule. Producing it in a clandestine lab would be extremely costly,’ says Margraf. Few counterfeiters would have access to sterile conditions for producing injectable drugs, either.
The shortages have also prompted compounding pharmacies to create their own versions of the drugs. Compounders are generally allowed to create bespoke formulations of some drugs for specific patients where there is a particular medical need (for example for children who need different dosages or to avoid allergies to certain ingredients). When a drug is in shortage, pharmacists may also be allowed to prepare compounded versions if they meet certain conditions.
In June and July, Novo launched legal action against several US medical spas, weight loss or wellness clinics and compounding pharmacies selling products claiming to contain semaglutide. In September, Eli Lilly began its own legal actions against compounded tirzepatide products.

In response to Novo’s assertions that compounding with semaglutide is prohibited, the Alliance for Pharmacy Compounding stated that: ‘FDA guidance on the compounding of copies of FDA-approved drugs when they are in shortage makes no distinction for a patented drug.’
Some compounding pharmacies may have accessed semaglutide from FDA-registered facilities, the alliance claimed, and Novo had not completely locked down the supply chain on the active pharmaceutical ingredient.
There’s tremendous frustration that there’s such a supply-demand mismatch
Nonetheless, the FDA drew attention to reports of some compounders using sodium or acetate salt forms of semaglutide, as opposed to the free base form used in the approved drugs. ‘Compounded drugs are not FDA-approved, which means they are not subject to premarket review for safety, effectiveness or quality,’ an FDA spokesperson noted.
‘[Some] compounding pharmacies are not quite following the letter of the law,’ says Margraf. ‘I think it’s a cash grab.’ Stanford stresses that she would never recommend compounded semaglutide to her patients. ‘We have no evidence that there’s any level of testing to demonstrate that these [compounded drugs] are the exact same agents,’ says Stanford.
Insatiable demand
With both Lilly and Novo seeking to demonstrate the health value of their drugs, it looks likely that demand – and hence pressure on the supply chain – is unlikely to ease anytime soon. Lilly’s tirzepatide produced impressive weight loss results in the recently reported phase 3 Surmount trials looking at using the drug to support longer-term weight management.
Meanwhile Novo has published data showing Wegovy can significantly reduce the risk of strokes, heart attacks and death in patients with established cardiovascular disease and classed as overweight or obese. The company suggests these benefits are not simply the result of weight loss, and has petitioned regulators to expand the drug’s label information to include heart benefits.
Analysts at JP Morgan estimated that anti-obesity drug revenues could climb to between $30 billion (£24 billion) and $100 billion by 2030. Meanwhile, analysis by Trilliant Health of GLP-1 prescriptions found that sales volumes rose by 300% from the start of 2020 to the end of 2022, with Ozempic accounting for 65% by the end of last year. Just over half of patients prescribed Ozempic or similar had a history of diabetes.
‘We haven’t seen anything like this before in terms of the rapid unfolding of quite compelling evidence,’ says Louise Baur, obesity researcher at the University of Sydney and president of the World Obesity Federation. ‘Suddenly there’s more trial results for these medications coming out and it is hard to keep up with all the rapid changes.’ She says doctors will need to get to grips with which medications work best with which patients and how to manage side effects and dosing regimens.
‘Our armamentarium for obesity has been really limited,’ says Baur. ‘Then along comes these medications and doctors are saying we can make a difference to our patients with obesity.’ She too has seen shortages of the GLP-1 diabetes and obesity drugs in Australia. ‘There’s tremendous frustration that there’s such a supply-demand mismatch,’ she adds. Her lean husband has been unable to get Ozempic to treat his diabetes, she notes.
However, GLP-1 mimics do have notable side effects – predominantly gastrointestinal, such as nausea, diarrhoea and stomach pains, which are more likely to happen when patients begin taking them or increase their dose, according to Cleveland Clinic. There have also been media reports focused on concerns around mental health, and the European Medicine Agency has initiated a review on the risk of suicidal thoughts and self-harm in patients taking GLP-1 medicines.
Expanding options
There are many more GLP-1 and related drugs in clinical trials. Pfizer is developing an oral GLP-1 agonist candidate (danuglipron), and reported positive results from a phase 2 study in May.
Meanwhile, Eli Lilly is moving forward with retatrutide for diabetes and obesity, which targets three receptors, including GLP-1. It has published positive phase 2 trials in the US and is entering phase 3 trials for obesity.
A dual agonist targeting GLP-1 and glucose-dependent insulinotropic polypeptide (GIP) receptors is also in the works from Viking Therapeutics. It is now conducting a phase 2 trial in patients with obesity. Amgen has completed a phase 1 trial with a dual agonist that includes GLP-1.
Both Lilly and Novo – buoyed with cash from sales of these drugs – have been buying up smaller biotechs with weight management prospects, and AstraZeneca has licensed a GLP-1 agonist from Eccogene.
‘There’s optimism now because there’s so many players coming to this space. We’re not just going to be relying on Novo or Lilly,’ says Stanford. She notes that the first GLP-1 drug, liraglutide – which was approved in 2015 – required daily injections and led to 5–6% average weight loss. Demand was relatively low.
‘There has been astronomically more interest in the new drugs,’ Stanford says. Weekly injections are more convenient, and the weight loss is more significant. However, with liraglutide’s patents expiring, cheaper generics will likely be available in 2024, which could see its use expand again.














No comments yet