Researchers are trying to understand how orexins influence our appetites, and whether we can use them to treat addiction and obesity, explains Andy Extance
To study how some little-known brain chemicals affect our eating behaviour, Robyn Brown’s team is trying to frustrate mice with chocolate. At the University of Melbourne in Australia, her team prepares mice by giving them access to sweets for two hours every three days. ‘That gets rodents very excited,’ Brown tells Chemistry World. Eventually, test day comes. ‘We put food in a tea strainer and dangle it in the home cage,’ Brown explains. ‘They can see and smell the food, but they can’t actually get to it.’ After stressing the mice in this way, the Melbourne researchers open the tea strainer. Then, some mice eat nearly two-thirds of their usual daily food intake in just 15 minutes.
Until now, Brown says, it was difficult to do experiments to work out what is happening inside brains in stress-induced binge eating. ‘Often when rodents get stressed, they’ll stop eating, just like some people will stop eating when they’re stressed,’ she says. ‘But there’s a portion of us – I’m one of those people – that get stressed out and overeat.’ Using her team’s new model, Brown hopes to study the role that signalling molecules most commonly called orexins might play in stress-induced binge eating.
The lessons Brown’s team learns from these tiny creatures could have outsized significance. The 2019 Health Survey for England found that 28% of the country’s adults were obese. The 2017–2020 US National Health and Nutrition Examination Survey found that 41.2% of adults in that country were obese. Brown underlines that a century ago, less than 10% of people were obese. ‘Genetics can’t change that quickly,’ she says. ‘So, it’s about how we’re interacting with our environment.’ Brown works with an endocrinologist who runs obesity clinics, which primarily treats metabolic issues, such as type 2 diabetes. ‘No one seemed to be focused on eating behaviour, which leads to obesity,’ she says.
That’s why Brown is interested in orexins. They differ greatly from molecules better known for their role in controlling hunger, the hormones ghrelin and leptin. While ghrelin and leptin circulate through our bodies, orexins are neuropeptides, acting only in our brains. Where ghrelin stimulates hunger and leptin suppresses it, orexins’ influences are more fundamental. Evidence suggests that orexins arouse us. They focus us on interesting opportunities around us, such as eating chocolate sweets, but also taking illegal drugs. Prescription drugs are already harnessing the orexins’ role in arousal. And now, researchers like Brown are seeking to understand and exploit how they affect our behaviours.
Finding the right key
Scientists discovered ghrelin, leptin and orexins in the 1990s amid growing concern about obesity. They were enabled by new molecular biological methods involving genetic modification, cloning and protein purification. Right from the orexins’ discovery in 1998, it was clear they had multiple roles. In January and February of that year, two teams first published details of their existence, coming from completely different angles.
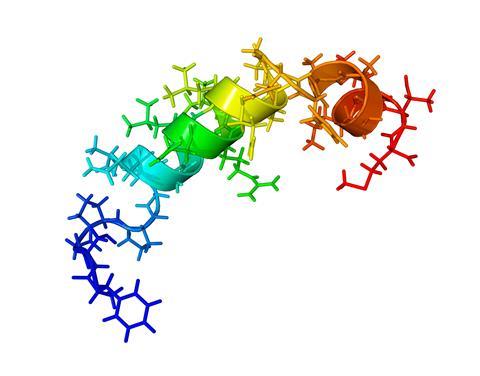
Masashi Yanagisawa’s team at the Howard Hughes Medical Institute (HHMI) in Dallas, US, were investigating a mysterious class of receptor proteins in human brains. Such receptors are usually thought of as ‘locks’ that turn when activated by smaller neurotransmitter molecule ‘keys’. Unlocking might trigger a nerve signal through a neuron cell, for example. The HHMI team knew that a receptor type existed that did not match any previously known neurotransmitters, explains Takeshi Sakurai from the University of Tsukuba, Japan.
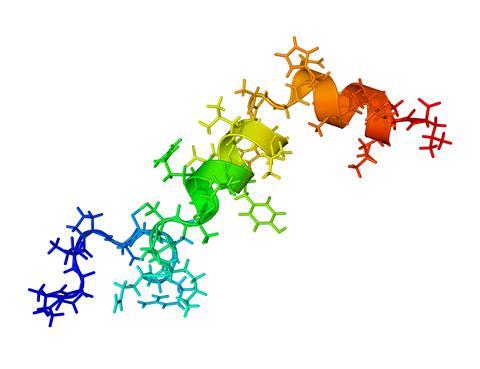
Then working at HHMI, Sakurai identified that two different peptides, which they later termed orexin-A and orexin-B, activated the receptors. The team then injected a synthetic version into rats’ brains, finding it increased food intake. ‘Feeding behaviour was a hot topic, so we focused on their function in regulating feeding behaviour,’ says Sakurai. They also discovered two types of receptors, called OX1R and OX2R. But when Yanagisawa presented findings at a conference, the team was surprised to discover another group presenting data on the same peptide chains.
Gregor Sutcliffe’s team at The Scripps Research Institute in California, US, had been looking for genes that only cells in one brain area turned into proteins. With his student Luis De Lecea and their colleagues, they focussed on the hypothalamus, considered a key control centre in the brain. Among the genes they found were those encoding the orexin peptides, but they called them hypocretins. Rather than feeding, the researchers noted a role in exciting nerves, a hint towards orexins’ best-known function.
Yanagisawa’s team and other scientists would later show that the peptides help regulate our sleep and wake cycles, with an absence of orexin-producing neurons being one cause of narcolepsy. Sudden paralysis or sleep are striking symptoms of orexin deficiency in humans, dogs and mice, says Denis Burdakov at ETH Zürich, the Swiss Federal Institute of Technology. More than one person in every 2000 suffers from such orexin deficiency, with positive emotions from winning a game, being tickled or eating chocolate causing these ‘attacks of cataplexy’. Orexin-deficient dogs pass out when given meat, for example.
Paying attention to feeding
While other researchers have mainly focussed on orexins’ sleep/wake function, Sakurai has been among those studying orexins’ connection to feeding. His team found that leptin potently inhibits signals passing through orexin neurons, while ghrelin excites them. Yet scientists are still deciphering those connections.
At a basic level, leptin reads out how much energy is in our bodies, explains Stephanie Borgland from the University of Calgary in Canada. ‘Leptin is released from your fat cells and circulates and suppresses appetite based on how much energy you have,’ she says. Specifically, fat cells release leptin when they take up lipid molecules, or when you’re sleeping. By contrast, stomach lining glands pump out ghrelin in response to stress and hunger, opposing leptin’s actions. We release these hormones – and orexins too – throughout the day as part of our circadian rhythms, Borgland explains. ‘Waking up in the morning orexin and ghrelin would motivate you to consume food,’ she says.
Borgland sees orexins as a motivator in part thanks to research from Gary Aston-Jones’ team in the US. In 2005, the group showed that orexin cells in the lateral hypothalamus motivated mice to seek cocaine and opioid drugs and tasty, sugary food rewards. Aston-Jones, currently at Rutgers University in New Jersey, US, says that since then many experiments have shown that OX1R, which can be activated by both orexin-A and orexin-B, ‘plays a critical role in motivation for many different drugs but also natural rewards’. His team combines this with sleep, waking and other roles in a general hypothesis called ‘motivational activation’ in which orexins are ‘an on switch for many different behaviours’.
Such findings suggest separation between energy-management hunger mediated by ghrelin and leptin and cravings suggested by cues around us. ‘You drive past a McDonald’s sign and even though you’re not hungry you feel like “I want to go have a hamburger”,’ says Aston-Jones. ‘That, I think, is where the orexin system gets engaged in particular.’ Blocking OX1R might then reduce those feelings without affecting more fundamental feeding circuitry. Aston-Jones also proposes that orexin neurons can have many different functions, depending on where exactly where they connect to.
Many orexin neurons start in the lateral hypothalamus, connecting to other areas all over the brain. The lateral hypothalamus is similar between different species, because it controls many basic brain functions, including feeding, sleeping and waking. With their widespread connections, Burdakov calls orexin neurons a ‘brain government’. One key brain area that they connect to is the ventral tegmental area (VTA). From the VTA, neurons activated by the neurotransmitter dopamine spread out to perform their own brain government role, although not as widely as orexin neurons. Dopamine is perhaps best known as a ‘feel-good’ chemical, for its role in pleasurable rewards and motivation. But in practice dopamine’s function is complex – and so too are orexins’ functions.
Feeling hangry?
Have you ever felt so distressingly hungry you felt angry, a combined emotion some call hangry? Stephanie Borgland from the University of Calgary in Canada notes that researchers have looked at intense hunger states that seem a lot like hangriness. Two different studies found that such states involve neurons in an area of the hypothalamus called the arcuate nucleus. Some of these neurons contain a neurotransmitter called agouti-related peptide (AgRP), and ghrelin can typically activate them. Borgland notes that orexin neurons connect to the arcuate nucleus and may also activate the AgRP neurons. She speculates that this ‘may drive aversive hunger states’.
While neither paper uses the term hangry, the University of Melbourne’s Robyn Brown has no doubt that the sensation is real, especially in children who have used up their energy supply. She thinks that sufficiently high ghrelin levels would be enough to cause the effect. ‘My God, the mood change from negative to positive energy balance is just so pronounced with kids,’ she says.
Ambiguous connections
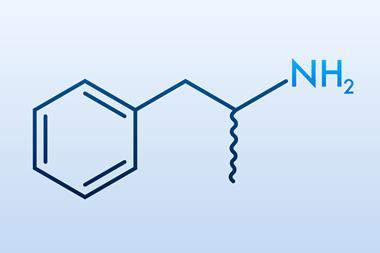
As well as responding to rewards, orexin neurons can also activate in response to threats and stress, particularly in the medial rather than lateral hypothalamus. OX2R is also more involved with stress responses and sleeping and waking than OX1R, says Aston-Jones, and therefore is the receptor that orexin inhibitors to treat insomnia should target, he explains. Three orexin antagonists already approved by the US Food and Drug Administration treat insomnia: suvorexant (sold as Belsomra), daridorexant (Quviviq) and lemborexant (Dayvigo) target both OX1R and OX2R, as Aston-Jones notes. Overall, he says that the hypothesis that orexins mediate reward-driven behaviour through arousal and motivation isn’t as well accepted as its sleep/wake role but is ‘gaining traction’.
One theory is that we eat to turn off orexin cells, because we do not like feeling anxious
Also in 2005, De Lecea’s Scripps team took a different view on how orexins drive motivation, pointing to stress as the primary factor, rather than rewards. Burdakov says that this has caused unnecessary arguments among scientists. ‘That paper showed that orexins cause stress-like states, and that leads mice to reinstate drug seeking,’ he explains. Likewise, orexins increase anxiety and are turned off by eating. ‘One theory is that we eat to turn off orexin cells, because we do not like feeling anxious,’ Burdakov says. ‘For me, it’s the same thing. If you’re stressed, you will seek rewards. The most frequent stimulus for relapse if you’re a recovering drug addict is that you get very stressed. Stress causes reward seeking, so the two are the same thing.’
As another puzzle piece, Sakurai likewise highlights that lack of orexins doesn’t dramatically change hunger. Orexin-deficient mice eat slightly less but, because they’re not as motivated, they run around less and gain weight because they burn less energy. Likewise orexin-deficient people tend to be a little overweight.
In 2009 Borgland untangled this complexity a little by looking at what exactly orexins were doing in the VTA. Her team found that it caused more NMDA receptors, which recognise the common neurotransmitter glutamate, to come to the surface of synapses connecting orexin neurons to their neighbours. That effectively amplifies any signals coming through glutamate neurons, Borgland says. Her team hypothesised that this made it more likely that we’d work harder for rewards like tasty food.
To test this idea, the Calgary scientists studied rats in a progressive ratio lever press test. In it, rats first get a reward if they press a lever once, then three times, then five times, increasing until they give up. They did this for normal rat food, high-fat chocolate pellets – and cocaine. Predictably, rats gave up more easily with a normal food reward. But surprisingly, blocking orexin signalling only changed how motivated rats were to get high-fat chocolate and cocaine, not their normal diet. That suggests that orexins only come into play for what mice really enjoy.
Orexin hacking
The findings show how orexins feed into dopamine motivational reward systems and connects food and drugs like cocaine. The reward system ‘isn’t for drugs of abuse, it’s to guide us to find cues in the environment that predict food’, Borgland says. ‘Drugs of abuse take advantage of that.’ As a result, researchers are now testing orexin antagonists like suvorexant in clinical trials as anti-craving and addiction treatments, and against binge eating, but not obesity. ‘The challenge is that people with obesity are not necessarily binge eaters,’ says Borgland. ‘There’s a lot going on in obesity.’
Orexins are highly regulated by circadian rhythms
Brown is likewise using what’s known about drug addiction to look at why people struggle with binge eating. ‘I was really interested in whether orexins could be involved in mediating this specific type of overeating behaviour,’ Brown says. She is now just beginning to explore this with her mouse-frustrating model of stress-induced binge eating. However, her discussions with drug companies to date suggest they have little interest in developing treatments for eating disorders and addictions. Instead, they are focussed on developing orexin drugs for insomnia because ‘they don’t have the abuse potential that some other sleep-promoting drugs do’.
Even if orexins’ influence on food and drugs proves to be consistently unattractive to drug companies, knowing how it functions could still help us. For example, it explains why good sleep and routine benefit most people, according to Borgland. ‘Orexins are highly regulated by circadian rhythms – when we sleep, when we eat,’ she says. ‘I would argue that getting a good sleep and eating when you typically eat is less likely to induce mass release of orexins which might arouse different systems and motivate you to eat or drink or make you stressed.’
Burdakov sees another opportunity after his ETH team found, like Borgland’s group, that orexins’ role could differ between foodstuffs. The researchers looked at different amino acids, fats and sugar, finding them to influence orexin neurons differently. Calories eaten as amino acids stimulated orexin neurons more than the same number of calories taken as sugar. What researchers have found out about how and why we enjoy food and drugs, and the consequences of that, so far has been tantalising. But the ETH team’s finding on food’s varying impact on this neurotransmitter alone has significant implications for the degree of control we have over our bodies.
‘Orexin neurons are a bit like your heart,’ Burdakov explains. ‘You cannot just say “OK heart, now beat at 92 beats per minute.” But you can accelerate your heart: you can drink a lot of coffee, for example. We’ve been exploring the same idea for orexins.’ It will take more research to work out whether avoiding sugary foods or eating non-essential amino acids in foods like tofu and eggs could prevent you feeling lethargic. But if they do, Burdakov argues that orexin cells’ dietary sensitivities could let people ‘expand the reach of their free will into the subconscious’.
Andy Extance is a science writer based in Exeter, UK











No comments yet