A bio-inspired approach to creating universal red blood cells
Chinese scientists are developing a new approach to create “universal” blood: red blood cells (RBCs) that can be transfused into any patient, regardless of the patient's or recipient's blood group.
Blood groups are characterised by the presence (or absence) of various proteins known as antigens on the surface of RBCs, the most well-known of which form the ABO system and the Rhesus D (RhD) system. One consequence of the existence of these groups is that blood mismatching can occur when an incompatible blood group is used for transfusion. The recipient’s antibodies recognise the antigens on the donor RBCs as being foreign and attack the cells – with potentially fatal results.
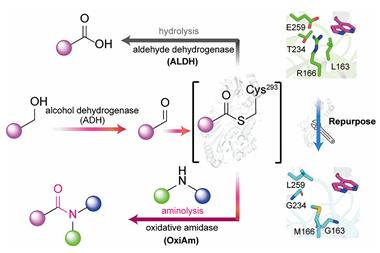
Several approaches have been investigated in the past to strip RBCs of their antigen identity, such as chemical cleavage of the antigens, disruption of antigen–antibody binding by grafted poly(ethylene glycol) molecules or ex vivo production of universal RBCs from genetically engineered hematopoitic stem cells, but each of these methods has its downfalls. Ruikang Tang and co-workers, from Zheijiang University, have used a simple method to mask the ABO group antigens by chemically modifying the RBC surface with polydopamine (PDA), a mimic of the bioadhesive produced by the mussel Mytilus edulis.
‘The concept is very clever because the coatings can be performed in situ using dopamine as a precursor molecule,’ says Christopher Bettinger, a biomaterials researcher from Carnegie Mellon University in the US. ‘The resulting polydopamine coating is therefore composed of materials that already exist in the human body.’
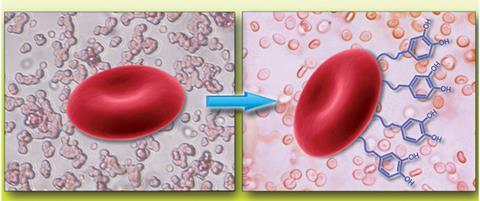
In vitro experiments using PDA–RBCs have shown that the antigenic response that occurs during blood mismatching is absent, while the structural and functional characteristics of the modified RBCs remain unaltered. Initial in vivo studies in mice have also shown that the modified RBCs behave in the same way as native cells, with comparable life spans and no sensitisation of the donor immune system, even after multiple transfusions.
The eventual aim of the work is clinical application. Having a stock of universal blood that can be transfused quickly in emergencies, or for treating people with rare blood groups where stocks are scare, would be an invaluable resource for medics. There are still hurdles to overcome, for example only the ABO blood group system has been demonstrated in this study; showing that the strategy can also be applied to the RhD system is essential. Tang, however, is optimistic and says it would be ‘pretty exciting’ if their approach was further developed for clinical trials.
References
This paper is free to access until 1 July 2014. Download it here:











No comments yet