Biogen abandoning Alzheimer’s antibody aducanumab is unusual, but hardly surprising
It’s not very often that you see a pharmaceutical company completely giving up on a drug that’s already won regulatory approval and has reached the market – at least not without uncovering some serious side effect that didn’t show up in the clinical trials. With many of the difficult, risky parts of the process already traversed, it should be time to sell some product and recoup some investments. And you wouldn’t have put all that effort into a product that you didn’t believe was going to be able to do that, naturally.

But it does happen. A famous example was Exubera, an inhaled insulin product. The idea was that this route would be so much easier and faster than self-injection that it would capture a good share of a very large market. Pfizer had convinced itself of this, and had convinced a number of financial analysts as well. So, it came as a rude surprise when the product absolutely flopped. Physicians weren’t particularly interested in prescribing it, and patients weren’t particularly interested in trying it. The company withdrew it from the market the very next year. In another example, some of the early drugs approved against Hepatitis C were also abandoned quickly due to overwhelming competition and vanishing revenues.
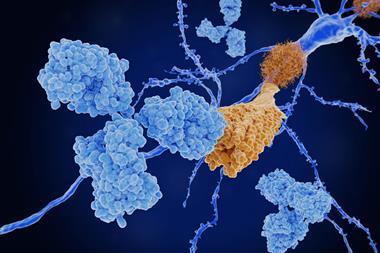
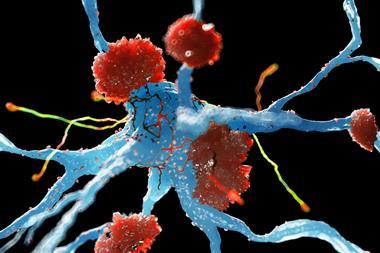
The newest example is Aduhelm (aducanumab), the anti-amyloid antibody developed by Eisai and Biogen, which was (in)famously approved by the US Food and Drug Administration (FDA) despite the objections of its own advisory panel and its own statisticians. The controversy was so great that Medicare (the state-backed medical programme for over-65s, and a huge customer for any Alzheimer’s drug) refused to pay for it unless patients were involved in another clinical trial to determine if the drug actually had any real benefit. You’d think that would be the sort of question you’d have cleared up before a drug hit the market, but for some reason the FDA decided that Everything Was Different Now.
Biogen announced recently that it is discontinuing Aduhelm, and this definitely wasn’t due to overwhelming competition. There was nothing else like it on the market, but very, very few physicians were prescribing it after Medicare and other large insurers balked. The drug was also never approved in Europe or elsewhere. Unlike Pfizer with Exubera, though, Biogen had another reason to give up on Aduhelm: it has, along with Eisai, another anti-amyloid antibody approved – Leqembi (lecanemab) – and they want to concentrate their resources on that one. Truth be told, the clinical data for it are not (in my opinion) much more compelling than Aduhelm’s, and there are safety concerns as well. Standard opinion in the drug business has been that the first effective drug against Alzheimer’s would surely be a record-setting success, but that word ‘effective’ is causing difficulties. It’s possible that the word ‘safe’ will also become troublesome; that will bear watching, too. The same concerns hold for donanemab – another antibody from Eli Lilly that is expected to be approved soon.
You can draw different lessons from Aduhelm’s failure depending on your prior views. Libertarian types have long championed the idea of approving drugs based mostly on safety, and letting the independent judgments of physicians and patients sort things out afterwards. Aduhelm certainly wasn’t approved on efficacy, so perhaps its failure at the hands of insurance (both public and private) is what the libertarians had in mind? But the heavy hand of the US government (in the form of Medicare’s rejection) surely spoils that story. You could also see the Medicare decision as the last line of defense holding against the effects of an unusually bad regulatory decision. From one perspective that’s heartening, but it really shouldn’t have to come to that. Medicare is not really designed as a drug approval mechanism. You can stop a car by overheating the emergency brake and steering into a wall of tyres, but that’s not a sustainable way to drive to work.
So the progress of the next two antibodies will be of great interest. My opinion is that if the amyloid hypothesis for Alzheimer’s were as strong as we used to think it was, then these drugs should have led to greater things. If you’d told everyone back in 1990 about their undeniable amyloid-clearing effects, the last clinical outcome you’d have expected would be everyone having to squint their eyes and turn up the room lights to see any sort of real-world effect. The world is still waiting for a good Alzheimer’s drug. I cannot begin to guess when it might arrive.















1 Reader's comment