Computer and mobile phone combo detects Chagas disease in blood and could drive down diagnosis costs
Scientists in the US have devised a new way of carrying out blood tests – based on a modified computer and camera phone – that could lower the costs of disease screening in developing countries.
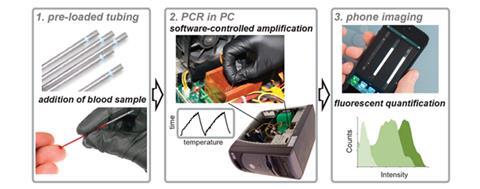
Their system uses the heat from the computer’s CPU to carry out a polymerase chain reaction (PCR), which amplifies pathogen DNA that then binds to a fluorescent probe. This can then be imaged using a camera phone, giving a fast diagnosis for a fraction of current costs. The team were able to detect DNA from Trypanosoma cruzi, the parasite that causes Chagas disease, in blood samples.
‘PCR is a well-developed molecular technique that has been applied to the detection of a vast range of infectious diseases; however, it has the drawback of requiring sophisticated equipment that is operated by trained personnel,’ says Tom Soh, who developed the system with colleagues at the University of California, Santa Barbara. ‘By repurposing existing technology, we keep the fixed costs to a minimal $41.50 [£25.40]. Conventional PCR has build-up expenses on the order of $20,000. That’s a 500-fold increase.’
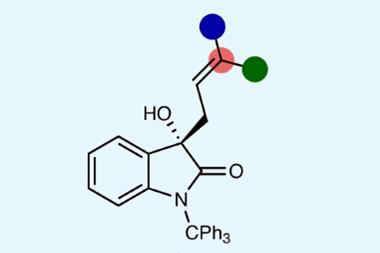
To carry out a test, the blood sample is loaded into a capillary tube with PCR reagents, including primers specific to the target sequence, a DNA polymerase enzyme and the fluorescent dye. The tube (with up to 28 others) is then placed between the heat sink fins of the CPU. Software is used to control the CPU temperature – one program heats it up by demanding high-power calculations, then another cools it down rapidly using the fan. These temperature cycles break the DNA strands apart then allow them to be copied by the polymerase enzyme, amplifying the target sequence. The DNA is then detected and quantified using a camera phone with a filter that allows it to image the fluorescent dye.
As a proof-of-concept, the team used their system to detect T. cruzi DNA in blood at levels comparable to those seen in Chagas disease sufferers. Soh says the technique could be used to diagnose other diseases whose genomes have been sequenced, including hepatitis, tuberculosis and HIV.
‘Using a PC heat sink for thermal cycling in PCR is a new idea,’ comments Ali Yetisen from Cambridge University in the UK, adding that the team have done ‘good work’. But he thinks the estimated cost saving is ‘grossly exaggerated’. ‘They leave out a significant amount of equipment they use in the analysis,’ he says. He also points out that any device that requires manual handling of reagents increases the risk of contamination, which can be off-putting for clinicians working at the point-of-care.
Soh admits there are improvements to be made to the system, and says the team are now focusing on getting it ready to use in the field. ‘The use of a laptop in place of the PC would reduce reliance on power sources and increase portability,’ he says.
References
F M Walker et al, Anal. Chem., 2014, DOI: 10.1021/ac5022419










No comments yet