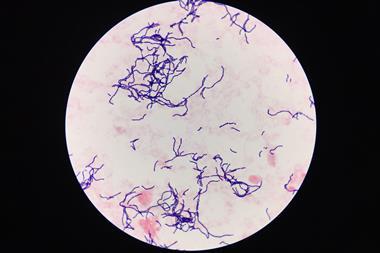
Researchers in India have shown that an amphiphilic molecule can enhance the bactericidal activity of obsolete antibiotics by helping such drugs accumulate within Gram-negative bacterial cells.
Antimicrobial resistance mechanisms in bacteria include reducing the permeability of their outer membrane and efflux pumps that extrude antibiotic drugs. The growing creep of drug-resistant infections means we are in urgent need of new antibiotics that bacteria have never encountered and lack a mechanism to resist. But drug development is slow and costly, compelling the scientific community to explore other ideas.
Administering an adjuvant molecule alongside an existing antibiotic is one such alternative. Some adjuvant molecules aid antibiotic delivery by permeabilising cell membranes and suppressing efflux pumps. But a notable drawback typically associated with these adjuvants is their lipophilicity. This characteristic enables antibiotics to pass through both bacterial and mammalian cell membranes, resulting in non-selective cell death.
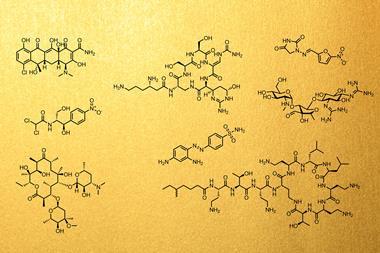
Now, Jayanta Haldar and colleagues at Jawaharlal Nehru Centre for Advanced Scientific Research (JNCASR) have designed and finely tuned the chemical make-up of a new molecular adjuvant to make it biocompatible with mammalian cells. Their adjuvant molecule features long hydrophobic chains to improve membrane permeability, accompanied by ethanol groups for amphiphilicity and to induce specific hydrogen bonding interactions with Gram-negative bacterial membranes.
Halder’s team initially tested their molecular adjuvant in combination with the antibiotics rifampicin, fusidic acid, minocycline and chloramphenicol before deciding to focus on fusidic acid. In a cellular assay, a combination of fusidic acid and the molecular adjuvant was effective against biofilms produced by Acinetobacter baumannii, a type of bacteria that is responsible for many drug-resistant infections. Not only did the adjuvant enhance membrane penetration, it also inhibited efflux pumps, allowing fusidic acid to accumulate within the bacterial cells. The combination did not appear to be toxic to mammalian cells and had potent antibacterial activity in a mouse skin infection model.
However, Halder’s lab did observe high lethality when administering the adjuvant intravenously to mice. The impact of this adjuvant on mammalian toxicity is therefore ‘still something to be discussed and debated’ says Nathaniel Martin, a professor of biological chemistry at Leiden University in the Netherlands. Another consideration for systemic application, says Martin, is the need for both molecules to locate the bacteria at the same time and place, requiring a match in their pKa profiles. Martin says that ‘this is an aspect that will need to be addressed and optimised’ in the future.
The research team at JNCASR acknowledges that devising a suitable delivery system for the adjuvant and antibiotic will be challenging. JNCASR team member Riya Mukherjee says they next need to perform in-depth mechanistic studies and pre-clinical efficacy tests. Mukherjee also mentioned the need for monitoring resistance development, as ‘although the combination therapy may be initially effective, there is always a risk of bacteria developing resistance over time’.
Despite the pitfalls, Martin says that ‘the use of adjuvants to tailor the properties of existing antibiotics … can definitely be part of the solution’ in the fight against Gram-negative superbugs.












No comments yet