From small acorns grow mighty oaks. And the seed that Emmanuelle Charpentier and Jennifer Doudna planted just a decade ago has grown mighty indeed. The gene-editing tool Crispr–Cas9 is poised to deliver enormous benefits in healthcare and agriculture. How these benefits will be shared with the world is still a work in progress, however.
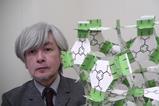
Crispr received a low-key reception from the scientific world when its repeating sequences of DNA were first spotted in a bacterial genome in 1987. Further investigation revealed that these repeating DNA sequences were part of a bacterial immune system targeted at viruses. Interesting fundamental science, but hardly something that could change the world it seemed. Yet early pioneers of Crispr spotted its potential and further work created a system that could both cut a genome at specific sites and insert new sequences.
Crispr therapeutics are now set to tackle some of the most intractable diseases. Numerous clinical trials are currently taking place, including eight just for sickle cell disease. However, the cost of Crispr treatments raises awkward questions about who will receive them. As Crispr therapies require sophisticated editing of cells, often outside the patient’s body, treatments are predicted to cost $2–3 million (£1.6–2.4 million) per patient. Health systems around the world are already under pressure from rising costs from drugs and ageing populations. Can even wealthy countries afford these treatments?
For the big killers like diabetes and cancer the answer is likely to be yes. The cost of treatment – should these therapies prove successful – will be offset by years of improved health and economic productivity. The cost of bringing the most sophisticated new drugs to market can exceed $4 billion, however. This means there is likely to be a hierarchy of diseases when it come to gene-editing therapies, with rare diseases without a big patient base set to lose out.
The good news is that technology can bring down these costs. Part of what enables Crispr therapies is genome sequencing. Its price per whole genome has fallen from $100 million in 2001 to less than a $1000 today. Automation of cell handling and gene editing could play a similar role in driving down costs. Governments and pharmaceutical firms should prepare now to avoid exacerbating health inequalities. A partnership between governments, industry, patient groups and others in the health sector could help ensure that rarer diseases are not forgotten. To deliver on Crispr’s transformative potential, no disease should be left behind.















No comments yet