Tiny delivery systems for cancer drugs
Encapsulating anticancer agents in nanoparticles can make them gentler on the rest of the body. Clare Sansom reports
Cancer drugs must target ordinary human cells that have been modified in various ways, picking up enough mutations to ‘go rogue’ and enter a state of uncontrolled cell division. The basic similarity between the cancer and normal cells remains, however, making it a difficult task to design a drug that is specific enough to kill tumour cells while leaving alone normal cells. First-generation cancer drugs are little more than cell poisons that target the mechanisms of cell division. This, however, also targets normal cell types that divide rapidly, including hair follicles, the cells lining the gastrointestinal tract and some types of immune cells – thus leading to characteristic side effects.
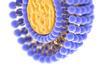
But if a drug can be delivered to tumour cells and to those only, then even one of the old-fashioned cell poisons that targets all rapidly dividing cells can become a safe, specific drug. And one way of doing this is to hitch the drug to its own miniature chemical delivery system.