Vaccines, probiotics and other substitutes could help battle antimicrobial resistance as antibiotic effectiveness fades
More attention must be directed towards vaccines and alternatives to antibiotics to combat the problem of antibiotic resistance. This is the conclusion of the latest report from the UK’s Review on Antimicrobial Resistance.

The new report, chaired by economist Jim O’Neill, says there is no guarantee that enough new antibiotics will be developed in time to tackle drug resistance. Other strategies such as vaccines, probiotics, immune stimulation and phage therapy must be considered. But we are not moving fast enough to develop alternatives, recognise their potential or use them appropriately, according to the report.
To renew impetus into vaccines and alternative approaches, the report says they should be included in the previously proposed $2 billion (£1.4 billion) global innovation fund for early-stage research. Existing alternatives should also be used more widely in humans and animals, with greater use of vaccines in the short term.
Universal coverage with a pneumococcal conjugate vaccine, for instance, could largely prevent the deaths of 800,000 children under five each year, O’Neill said. It could also prevent over 11 million days of antibiotic use in these children, reducing the development of resistance.
While some new vaccines are highly profitable and should not require public money to support them, others may not be commercially attractive. Any incentives created must be carefully tailored to each market and product, the report notes. And patients and doctors could be incentivised to use treatments that prevent future illnesses or resistance in society at large.
A recent review of potential alternatives to antibiotics identified 19 areas being worked on.1 ‘These are genuine opportunities to provide new ways to treat patients with infection and there is much more opportunity than there is capacity and funding to evaluate them in a timely manner,’ says Lloyd Czaplewski, first author of the review and director of Chemical Biology Ventures. ‘It is not all gloom and doom. There are things we can try, but we don’t know if they will work. The next 10 to 20 years is going to be a grand experiment to see if these alternatives can replace antibiotics or help them last longer.’
‘I blame big pharma for dropping the ball and putting us in this situation,’ says Vincent Fischetti, research bacteriologist at Rockefeller University, New York, US. ‘Clearly because of the neglect for decades, more research is needed into the immunology of disease and understanding the mechanisms of resistance by the organisms. Without this information, better strategies cannot be developed.’
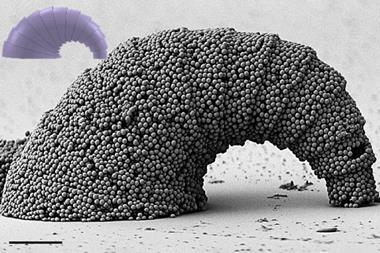
‘We were the first to use phage lysins as therapeutic agents 15 years ago, and it took this time for it to be accepted as a viable alternative and has now successfully completed phase 1,’ notes Fischetti. ‘So these “new” approaches take time to be accepted and developed. Many people are going to die needlessly because of this delay.’
The area needs to be treated in the same way as other big science projects, like the Large Hadron Collider or space exploration, Czaplewski says. And he says that the term ‘alternatives’ is a lead weight that needs to be jettisoned. ‘If these are successful they won’t be alternatives. They will just be different.’
This is the latest in a series of reports by the Review on Antimicrobial Resistance, before final recommendations are made to the UK prime minister in May 2016.
References
1 L Czaplewski et al, Lancet Infectious Diseases, 2016, DOI: http://dx.doi.org/10.1016/S1473-3099(15)00466-1







No comments yet