The molecular basis for the anti-inflammatory properties of cannabidiol (CBD) has been discovered that suggests that the compound not only inhibits inflammation but also helps to resolve it. The researchers say the insights gained could lead to new therapeutic strategies for treating inflammatory diseases.
Cannabis and cannabinoids, especially CBD, are well-recognised anti-inflammatory agents that are increasingly popular for treating inflammation-related disorders such as inflammatory bowel diseases and skin disorders. However, although several potential modes of action and molecular targets have been proposed, the exact mechanism by which they work is yet to be confirmed.
The researchers studied how eight different cannabinoids, including CBD and the psychoactive tetrahydrocannabinol (THC), act on human immune cells. All had anti-inflammatory effects and were found to inhibit the formation of pro-inflammatory messenger substances in cells while enhancing the formation of inflammation-resolving substances.
However, they discovered that CBD was the most potent anti-inflammatory of the cannabinoids and decided to investigate the compound in more detail.
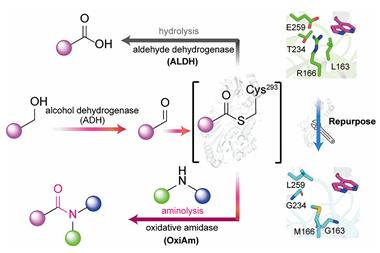
They were able to determine that CBD acts as a potent lipid-mediator class-switching agent in innate immune cells, shifting the formation of pro-inflammatory compounds, such as leukotrienes and prostaglandins, to inflammation-resolving specialised pro-resolving mediators (SPMs). These SPMs are potent endogenous anti-inflammatory compounds that function in host defence, pain and organ protection.
Their analysis showed that CBD directly suppressed formation of a leukotriene while also activating a lipoxygenase enzyme, triggering a change from pro-inflammatory molecules to inflammation-resolving SPMs.
The researchers were able to confirm that cannabinoids suppressed leukotriene formation and increased SPM production in a mouse model of peritonitis.
Currently, the major therapeutics to treat inflammation-related diseases are glucocorticoids and non-steroidal anti-inflammatory drugs. However, while these agents dampen inflammation and immune responses they fail to promote inflammation resolution, and they also frequently cause severe side effects. The researchers therefore said the mechanism of action exhibited by CBD represented an ‘alternative strategy with potential for pharmacotherapy of unresolved inflammation’.
‘This favourable biosynthetic shift from pro-inflammatory [lipid mediators] to inflammation-resolving SPM might be a plausible mode of action underlying the well-recognised anti-inflammatory properties of CBD and represents a molecular strategy to accomplish a local environment that is beneficial to promote inflammation resolution,’ they concluded.
Charles Serhan, an expert in infection and immunity at Harvard University in the US, describes the study as a ‘very important contribution’ as it brings together the cannabinoid field and the lipid mediators that play a role in the resolution of inflammation.
‘The group provides a mechanism for how the cannabinoids could evoke their well-known anti-inflammatory actions,’ he adds. ‘They clearly demonstrate that CBD switches off the pro-inflammatory mediators, the prostaglandins, produced by human M2 macrophages, and turns on the pro-resolving [mediators].’
But he said the ‘critical question’ was whether this can be demonstrated in a human trial. ‘A study like this will open the door for that possibility,’ he says.
Clive Page, an expert in the pharmacology of inflammation based at King’s College London, says it is increasingly recognised that CBD is not just a compound that affects cannabinoid receptors but has activity on a wide range of receptors.
‘The interesting thing [in this study] is that CBD is switching to the production of molecules that actually resolve the inflammation; that’s what happens physiologically…it’s when it doesn’t resolve that you end up with chronicity.’ Page agreed with Serhan that placebo-controlled trials of CBD in the clinic are now needed.
‘What we desperately need, and what is missing from the literature, is proper evidence in clinical trials…this paper effectively just adds more to the literature that we should be taking CBD seriously because, unlike THC from cannabis, it doesn’t have psychoactive effects and… it’s got a reasonable safety track record,’ Page adds. ‘What we’ve got to do is tease out the right dose for the right indication.’
References
L Peltner et al, Cell Chem. Biol., 2023, DOI: 10.1016/j.chembiol.2023.08.001















No comments yet