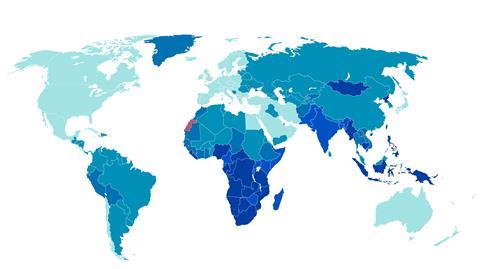
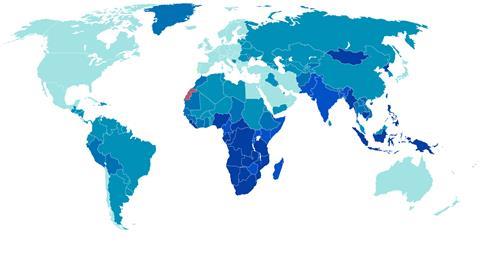
Many people around the world are either unable to afford the drugs they need, or their conditions have not been addressed by pharma R&D. Sarah Houlton investigates
The availability of modern medicines has driven dramatic improvements in human health, which are enjoyed by many of us living comfortably in developed countries. Yet there are many patients for whom treatment options are limited, whether that is because there are no drugs that treat their disease, or they cannot get access to those that do exist. In both cases, these are particular problems in the developing world. What is being done to address these concerns?
Katey Owen, director of the neglected tropical diseases (NTD) team at the Bill & Melinda Gates Foundation cites HIV, TB and malaria as three big infectious killers where the market has failed, and where her organisation is providing funding. ‘These diseases impact huge swathes of people who cannot afford to pay for medicines,’ Owen says. ‘So there is no incentive for drug development because there is no profit.’
While good progress has been made in the control of many of these diseases, there remains a stark contrast between the number of drugs in development for illnesses that affect high-income countries, and those only found in low- and middle-income countries. ‘Very big markets encourage R&D,’ says John Reeder, director of the World Health Organization’s special programme for research and training in tropical diseases (WHO TDR). ‘Could the problem be addressed by doing things a little differently?’
Collaboration
The advances that have been made in recent years have been due, in large part, to a collaborative approach to research, with academic groups, big pharma, public and private funders and product development partnerships (PDPs) all playing to their individual strengths.
‘All our work is done in collaboration,’ says Paul Wyatt, head of the drug discovery unit at the University of Dundee in Scotland. Its furthest advanced project, a clinical candidate for malaria that is about to enter Phase I trials, started with a library screening programme on a target identified by a partner, supported by the Medicines for Malaria Venture. ‘MMV funded our medicinal chemistry and design,’ he says. Subsequent activities have been carried out in collaboration with MMV and its partners around the world. A programme in visceral leishmaniasis and Chagas disease, meanwhile, is funded by the Wellcome Trust, and is a collaboration with GlaxoSmithKline.
Wyatt is clear that collaboration is the way forward. ‘You can try and do it alone, but the breadth of studies required makes it very difficult,’ he says. ‘You need disease experts in basic organism biology, but also parasitology, bacteriology, clinical experts, the ability to run assays, chemistry design, phenotypic screens for target identification, and so on.’
Funders play a vital role. First and foremost, Owen says, the Gates Foundation contributes money, but she believes this alone is not sufficient. ‘We also offer technical support, and many of our 1500 employees are folks who have come from careers in industry with technical backgrounds,’ she says. Those who are being funded often have an idea about what they want and how to get there, but technical partners can help to flesh out a workable plan, she says.
The foundation strives to find the best partners to address specific problems. ‘This is where the pharmaceutical industry comes in, as they are the best entities for developing new medicines for diseases,’ Owen says. ‘Whether that is vaccines or small molecule drugs, pharma’s model has proven itself effective, efficient and timely in achieving the reality of getting new chemical entities and vaccines onto the market. This is why we co-invest with pharma: they have the capabilities to solve the problems.’
PDP model
Funders such as Gates and Wellcome have been instrumental in the success of the disease-focused partnerships that have been pioneering research on drugs for neglected patients. Organisations such as MMV, the TB Alliance and the Drugs for Neglected Diseases Initiative (DNDi) enable research and foster collaboration.

DNDi is, first and foremost, a product development partnership, according to its R&D director Graeme Bilbe. He explains that a target product profile should be established at the outset, for each disease, to ensure the therapies can be used in the real world. ‘They will probably have pretty good stability for up to five years in extreme environments, such as the middle of Sudan where the temperature can be 55°C in the middle of summer,’ he says. ‘It should be easy to take, which usually narrows it down to a pill, though we do not rule out injectables.’
With the profile in hand, along with a good scientific understanding of how they might approach discovering and developing an orally active pill for the disease, they apply for money from bodies like Gates, Wellcome and government funding agencies.
Assets and expertise provided by pharmaceutical companies on an in-kind basis are invaluable. These can range from access to compound libraries and screening, to assistance with registration and holding product licences, as well as manufacturing and distribution. ‘It means we don’t have to go into the business of holding licences, doing pharmacovigilance or negotiating with WHO how much of the drug to produce each year,’ Bilbe says. ‘Industry has been honing its business for a long time and they’re the best in the world at this. It’s as good as getting money. We see our role as decoupling the costs of R&D from the process of bringing in cheap drugs.’
Company models
Several pharmaceutical companies have specific research initiatives focused on neglected patients, such as the Novartis Institute for Tropical Diseases (NITD). It is in the throes of relocating its efforts in parasitic diseases from Singapore to the US, where it will be co-located with its antibacterial and antiviral groups in Emeryville, California. ‘Novartis has a long-lasting commitment to malaria and we have two candidates in Phase IIb clinical trials,’ says NITD’s head Thierry Diagana. ‘We also hope to design new combination therapies that can tackle drug resistance.’
More recently, Diagana says, the company has started looking at cryptosporidiosis, a leading cause of paediatric diarrhoea for which there is currently no therapy. ‘The cryptosporidium parasite is closely related to malaria, and we’ve been able to advance a very interesting potential drug candidate,’ he says.
Partnerships have been a key element in how NITD has operated since its outset. ‘We cannot pretend that we can do this alone,’ he says. The partners complement each other, Diagana believes, with other organisations better placed to carry out a range of roles from delivery to monitoring drug resistance, he claims. ‘We need all those parts working together to advance drug candidates.’
GSK is doing something rather different. Its site in Tres Cantos, near Madrid in Spain, became the Open Lab Foundation in 2010, offering GSK facilities to external academics to pursue their projects. ‘We make sure there is a good fit between what the academic wants to do and what we can offer locally,’ says Lluis Ballell-Pages, the lab’s head. ‘It works as a nexus of collaboration with other pharma, with academic organisations and not-for-profits.’
We cannot pretend that we can do this alone
Thierry Diagana, head of the Novartis Institute for Tropical Diseases
At any given time, there are between 10 and 15 academic projects within the lab. ‘Between 80 and 100, mostly postdoctoral, scientists from academic institutions have worked at Tres Cantos,’ he says. GSK scientists get involved in the projects, too. ‘The idea is not just to host academics at our facilities: each project has a dedicated GSK mentor. It allows the basic science and drug discovery know-how of industry to be applied to academic ideas.’
There have already been some successes. ‘A number of lead optimisation programmes have been transferred into different units, some in GSK and some elsewhere,’ Ballell-Pages says. One project is now in Phase IIa, and there are several preclinical candidates.
As projects move into Phase III trials, where the cost is much higher, that partnership with external organisations will become ever more important, he says. ‘We know how to discover and develop molecules, but we cannot take on the full economic burden all the way,’ he says. ‘There are organisations who can help with these aspects, and then in the innovation part, the academics are important in order to feed the pipeline. There are three partners working together. It’s not simple but, in a way, it makes up for the market failure.’
High prices
The second gap is where products exist, but their high prices put them out of reach of many who might benefit. There has been great success with HIV drugs, but the same problem recurs in other diseases: expensive new treatments are neither affordable nor accessible to anyone other than the richest, says Katy Athersuch, medical innovation and access policy adviser at Médicins sans Frontières (MSF). ‘We are back to fighting those same battles all over again – what discounts are available for which country, and what licensing can be used to get generic access,’ she says.
An MSF project supplying new direct acting antivirals for hepatitis C in Cambodia is a case in point. ‘Because the number of people in the population in need of treatment is very large, and the cost of the therapies and the ability to provide care is not there, [local providers] are not able to meet this need,’ she says. ‘We see patients queueing to get access through us.’ The result is long waiting lists and rationing. Cheaper medicines could have a huge impact.

The success in HIV is in large part a result of the Medicines Patent Pool, set up by global health initiative Unitaid in 2010, which works within the existing industry business model to get medicines to neglected patients. ‘TRIPs [the World Trade Organization’s agreement on trade-related aspects of intellectual property rights] introduced patenting in various countries where it hadn’t existed before, particularly product patents in India,’ explains Greg Perry, MPP’s executive director. With product patents newly in place, Indian generics companies were unable to manufacture low-cost copies for the poorest countries.
Pharmaceutical companies have granted licences for patent and data exclusivity exemptions to generics companies via the pool, allowing them to supply the developing world with HIV medicines. The system has worked – Perry says that 94% of people living with HIV in developing countries now receive antiretroviral medicines, and all major products are included.
More recently, MPP has recently licensed several medicines for hepatitis C using a similar model, and is working on TB, which is necessarily very different. The use of new drugs in TB requires caution to discourage resistance, but the MPP model is based on high-volume generic uptake. They are therefore trying to address the issue at an earlier stage in the development process via the 3P, or ‘push, pull, pool’, project with MSF and various TB-focused agencies. ‘In TB, we are looking further upstream, in order to help and encourage drug development, and later, when it’s needed, we will also look at generic manufacturing,’ Perry says.
The WHO’s essential medicines list is a good starting point for looking at other disease areas, Perry says, and a feasibility study is being funded by the Swiss government. However, patents on most of the products on this list have either expired already or will do so soon, and therefore the added value of voluntary licences will be limited in these cases.
BiDiL
The heart drug BiDiL (isosorbide dinitrite/hydralazine) represents a drug for a different type of neglected patient: black patients with heart disease. The drug – a combination of two generic products – was developed in the 1990s by cardiologist Jay Cohn for the treatment of heart failure, but was rejected by FDA as its effectiveness was not statistically significant.
However, there were signals that it might be more effective in African Americans, a patient group for which antihypertensive ACE inhibitors are generally less effective. The license was sold to a new company, NitroMed, and a clinical trial on subjects who self-identified in that ethnic group was carried out that did show statistical significance. FDA approved the drug in 2005 solely for black patients on the strength of this trial.
The concept of a drug for the black population proved controversial. It was welcomed by bodies such as the Association of Black Cardiologists, which had been involved in the clinical trials, citing the tendency of African Americans to have stiffer blood vessels with a greater inclination towards higher blood pressure, and worse responses including more heart and kidney failure. Criticisms included the absence of patients of different ethnicities in the trial as a control, and wider concerns about the medicalisation of race. Sales were poor and NitroMed failed, but BiDiL was picked up by Arbor Pharmaceuticals, which still sells it today.
Corporate social responsibility
Patent pooling represents one way in which big companies can meet their corporate social responsibility goals. NTD treatment is heavily reliant on medicines donated by pharma companies, and Reeder says there has been a shift in recent years as many big companies recognise how important social responsibility is. Donation schemes for medicines for neglected diseases have underpinned various elimination campaigns. An early success was with Merck Sharp & Dohme’s veterinary antiparasitic medicine ivermectin, which the company has been donating to treat river blindness for 30 years. There are many other examples.
Ballell-Pages believes that if the pharmaceutical industry only focused on patients in the west, it would be doing the world a disservice. ‘Society gives us a licence to operate, but that comes with terms and conditions,’ he says. ‘GSK believes that one of those conditions is to put our capacity at the service of developing medicines for diseases of the developing world.’ An added bonus – though by no means the main driver – is that by addressing the more acute needs of patients in the developing world, it can give an understanding of the market for more traditional for-profit indications, he says.
New discovery models
The incentives for bringing new drugs to market in the developed world revolve around market exclusivity and patents, and therefore the ability to charge enough to recoup development costs and turn a profit. ‘This incentive is very good at steering innovation in particular areas, but it comes with the caveat that we have high prices,’ MSF’s Athersuch says.
Pharmaceutical companies are shareholder-owned, and therefore one of their primary motivations is to make profits and provide good returns for those shareholders. This is, clearly, at odds with the requirements of neglected patients, and Athersuch believes that the onus must be on governments to offer the right incentives.
Even when we are treating refugees in Europe, we are faced with European prices
Katy Athersuch, Médicins sans Frontières
‘I would put the emphasis on governments to take responsibility, and to put in place a framework that allows businesses to respond to it,’ she says. ‘The action I think companies can take is to openly embrace these new models, and engage on a serious basis. Yes, their primary responsibility is to shareholders, and they exist to make a profit, but they don’t have to thwart efforts to meet patient needs, and they should be part of the conversation on the alternatives.’
One idea involves giving cash prizes for successfully getting a product onto the market. The medicines could then be sold on a competitive basis, in the same way as generics are already – and in every country. ‘Even when we are treating refugees in Europe, we are faced with European prices, and have to ration who we can treat based on a product price that pays for R&D through the sale of individual pills,’ Athersuch says.
Whether or not a new model can be devised and gain widespread acceptance, there have been some positive moves, and the response to the Ebola and Zika crises shows that there is some will out there to develop treatments to emerging threats in the developing world.
But neglected diseases do not gain as much media attention, Reeder says. ‘It isn’t an either/or situation for me,’ he says. ‘We shouldn’t forget to invest in some of these really large problems that don’t catch the news. The fact the debate is going on is good. But if we look at the pipelines for these diseases, they represent a really small amount of the global drug R&D investment. We really need to address that inequity.’
Sarah Houlton is a science writer based in Boston, US












No comments yet