Condensing timelines from years to months inevitably involves compromises
The global rush is on to find a safe and effective vaccine against Covid-19. Experts and companies claim one could be on the market in 12–18 months. The US president wants one by the end of the year. According to the World Health Organization (WHO), 17 candidates are in clinical trials, with one already in Phase 3 and two others likely to enter in July.
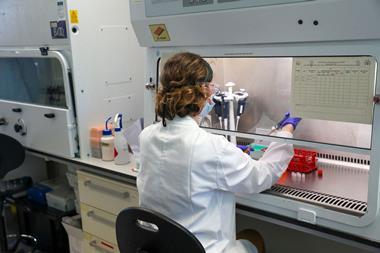
The accelerated speed of development has public health experts concerned that vaccines might be approved with incomplete data and analysis. At least one candidate has skipped animal testing, for example. Meanwhile, in China, CanSino Biologic’s experimental Covid-19 vaccine has been approved for the country’s military before Phase 3 trials have finished.
The concern intensifies when no vaccine against a coronavirus has ever been approved before, while many of the vaccine platforms in development against Covid-19 are unproven new technologies. ‘Developing a vaccine in about a year is unprecedented,’ says Byram Bridle, a viral immunologist at the University of Guelph in Canada, who has received Covid-focused funding to develop a new vaccine platform. ‘As a scientist with expertise in the field I am personally concerned that conducting science too fast could risk compromising the rigour needed to properly assess vaccines. A vaccine that is ineffective and/or unsafe will not be useful.’
Among the top concerns is the potential that a fast-tracked vaccine will have unintended side-effects. No vaccine is 100% safe, but if a billion people are vaccinated, a one in 10,000 serious adverse event will affect 100,000 of those people. In May, it was revealed that four out of 45 people in Moderna’s Phase 1 vaccine trial experienced ‘medically significant’ adverse events.
The most important thing is that fast tracking does not mean a compromise on safety or efficacy
Katherine O’Brien, WHO
In the upcoming Phase 3 trials, there will be up to 30,000 participants. But reliably identifying a one in 10,000 adverse event requires testing 38,500 people. Rarer events need even larger trials, explains Gregory Poland, director of vaccines research at the Mayo Clinic in Minnesota, US. ‘We won’t know about rare events until after the vaccine is licensed.’
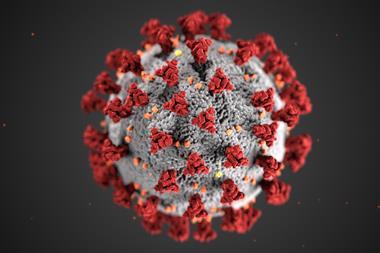
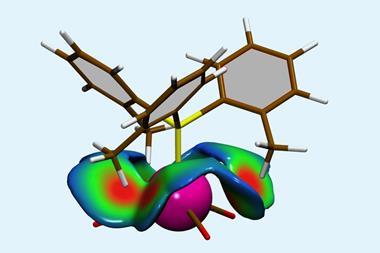
One potential adverse event is antibody-dependent enhancement (ADE), a type of immune reaction where vaccination makes subsequent exposure to the virus more dangerous. The condition – which has been observed with vaccines for measles, respiratory syncytial virus and dengue virus, as well as in animal models for the original Severe Acute Respiratory Syndrome (Sars) virus – occurs when the body, primed by a vaccine, generates antibodies that don’t sufficiently neutralise the virus when later exposed to it and instead encourage the virus into cells to replicate, exacerbating the disease.
According to Bridle: ‘There is definitely a risk of ADE; how much of a risk cannot be stated with any certainty though.’ Yet the US National Institute of Allergy and Infectious Diseases’ (NIAID) Vaccine Research Centre, which is collaborating on Moderna’s vaccine, has downplayed the possibility of ADE in a Covid-19 vaccine. Barney Graham, deputy director of the unit, told Proceedings of the National Academy of Sciences that because the Sars-CoV-2 coronavirus is structurally different to the cases where ADE has been seen, he doubts similar activity would apply.
How long would it take to determine if a vaccine can confer immunological memory for one year? Of course, it would take at least one year
Byram Bridle, University of Guelph, Canada
Regardless, Bridle says developers need to carefully assess the type of immune response their vaccines induce and test the response in vaccinated animal models exposed to the virus to ensure ADE does not occur. Poland has expressed concern that animal studies may not be completed before moving to human testing, which transfers extra risk to humans. However, he says that vaccine developers can’t really mitigate for side effects, apart from making sure the vaccine doesn’t contain amino acid sequences similar to human proteins and that the vaccine induces a balanced immune response.
To allay safety fears, the US Food and Drug Administration (FDA) released guidance at the end of June stating that nonclinical safety studies are necessary for novel vaccines and drug companies will be required to monitor their vaccines after approval. The WHO’s director of immunisation and vaccines, Katherine O’Brien, says fears of cutting corners are unfounded: ‘The most important thing is that fast tracking does not mean a compromise on safety or efficacy.’
Making memory
However, there is still a lot we don’t know about coronaviruses, which is another concern with speedy vaccine development. For example, the question mark over immunity – are antibodies protective and how long does immunity last?
Bridle says fast tracking vaccines risks compromising assessments of immunological memory. ‘Arguably, a vaccine against Covid-19 should confer immunity for more than one year to reduce the risk of future recurrences. But how long would it take to determine if a vaccine can confer immunological memory for one year? Of course, it would take at least one year. So how does that fit into the goal of getting a vaccine into broad public use in under a year? A prophylactic vaccine is useless if it does not confer long-term immunological memory’ to respond when exposed to the virus.
In addition, a fast-tracked vaccine may not be particularly effective. Bridle notes that the goalposts for success have already shifted from the search for a vaccine that protects against disease to one that merely reduces disease severity. The risk, says Bridle, is that poor-quality vaccines could potentially turn people into asymptomatic carriers that spread the virus.
At the end of June, Anthony Fauci, the White House health advisor and NIAID director, said the US was unlikely to develop herd immunity as a vaccine would potentially be only partially effective, adding he would be happy if a first vaccine was only 70%–75% effective. A day later the FDA released its vaccine guidance saying a vaccine would only need to be 50% effective in a placebo-controlled trial: an efficacy similar to the annual flu jab. Response has been mixed, with some experts saying the 50% figure is too low and others saying it is too high.
O’Brien says the WHO hasn’t specified the minimum effectiveness of a Covid vaccine, calling the determination complex ‘but there are certainly arguments for an efficacy lower than 50%’. She says as long as trials can enrol participants quickly and take place in areas where the disease is circulating then efficacy can be established in less than 12 months.
Maintaining confidence
Ensuring a vaccine is safe and effective will be essential in keeping the public’s trust in vaccines. There is a risk a fast-tracked vaccine could dent this and compromise vaccination programmes. Already in the US, around 30% of the public say they would reject a covid vaccine, according to various surveys. Poland says policies have to be driven by the science and effectively communicated to the public.
But with economies flagging from the health crisis, will society accept more risk in a vaccine? Bridle acknowledges this could be the case with Covid-19. Poland says the risk–benefit ratio of all vaccines will be carefully reviewed by authorities but notes risk boundaries are subjective.
O’Brien notes that trials will be halted either when a safety event is flagged or when the vaccine is found to be effective but ‘we can’t hold back an effective vaccine and forgo the benefit of it in the short-term in a pandemic situation just to wait for long-term safety evaluations’. Safety monitoring will continue after approval anyway, she adds.
But safety and efficacy concerns aside, there is more at stake here. Covid-19 won’t be the only coronavirus pandemic in the future, Bridle explains. The risk is we don’t build on the scientific gains once this pandemic recedes and we fail to use the data and technology to be ready to develop a safe and effective vaccine for the next coronavirus. Without funding, he says, this could be a real possibility.








No comments yet