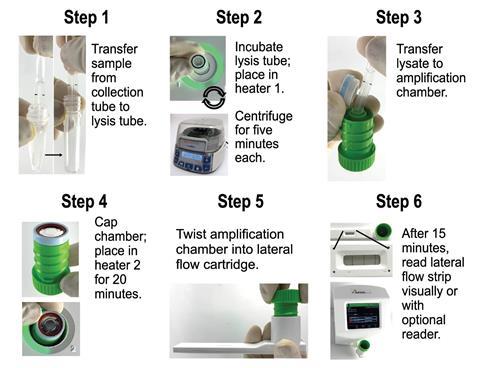
A new point-of-care assay to detect human papillomavirus (HPV) DNA requires just six user steps, gives results in under 45 minutes and costs less than $5 (£3.90) per test. Its developers hope it can fill a critical gap in resource-limited settings where the HPV rates are highest.

Despite the existence of a highly effective HPV vaccine and other prevention methods, cervical cancer continues to burden healthcare systems significantly, particularly in low- and middle-income countries. Directly detecting viral DNA using nucleic acid amplification tests is more effective than cytological methods such as Papanicolaou tests, also known as pap smears. However, the availability of equipment, reagents and trained personnel, and the associated costs, have posed a challenge to implementing these methods in resource-poor environments.
A multidisciplinary team of researchers led by Kathryn Kundrod and Rebecca Richards-Kortum from Rice University in Texas, US, has attempted to address this global disparity by developing an affordable and simple HPV DNA test. Their technique tests cervicovaginal swabs for the two types of HPV DNA that account for over 70% of cervical cancer cases, HPV16 and HPV18. It avoids the need for temperature cycling by using recombinase polymerase amplification instead of polymerase chain reaction. The time and cost associated with processing samples are reduced by using recombinase enzymes to separate DNA strands instead of heat.
After amplification, each DNA copy contains two antigens that are then captured on a lateral flow test that ‘works just like a rapid covid test’ according to Kundrod. The test features three signals – a control line that captures streptavidin-conjugated gold nanoshells that are added to the patient sample pre-amplification, and two HPV lines with anti-fluorescein and anti-digoxigenin antibodies for HPV16 and HPV18 respectively. The disposable test cartridges are designed to prevent workspace contamination that can lead to false positive results.
The scientists tested their assay in both a high-resource setting in the US using samples collected by a healthcare provider, and also a low-resource setting in Mozambique using patient-collected samples. While both trials demonstrated a clinically relevant limit of detection, the self-collected samples showed an increased cellularity that diminished assay performance. ‘Further work is needed to improve sample preparation for these types of samples,’ explains Richards-Kortum. ‘We think it illustrates why it is so important to include test evaluation in low-resource settings at an early stage.’
‘Self-collected samples are something that’s really something of interest in the field,’ says Jacqueline Linnes, who researches point-of-care diagnostics and global health technologies at Purdue University. ‘It’s much more private for the patients.’ This resonates with Kundrod and Richards-Kortum’s observation that over 90% of patients in the study’s Mozambique cohort chose to self-collect.
The next steps for the team are ‘to improve sample preparation and expand the number of HPV types included in the assay’ says Richards-Kortum. However, Linnes notes that this will be no small feat. ‘Whenever you’re multiplexing, there’s a chance that your primer sets are going to cross react, and then you’ll end up with false positives when you’re just throwing more things into that soup,’ she notes.
References
K A Kundrod et al, Sci. Transl. Med., 2023, DOI: 10.1126/scitranslmed.abn4768
















No comments yet