Propellants in asthma inhalers produce greenhouse gas emissions equivalent to driving 200 miles, yet most healthcare systems overlook this climate impact. New low-carbon alternatives are in development, Andy Extance reports, but barriers remain
- High climate impact of MDIs: Metered dose inhalers (MDIs) use propellants with high global warming potential (GWP), making them a significant contributor to healthcare-related emissions – one inhaler can equal the emissions from driving 200 miles.
- Industry and regulatory response: Pharmaceutical companies like AstraZeneca and GSK are developing inhalers with low-GWP propellants (eg HFO-1234ze, HFC-152a), driven by environmental regulations such as the Kigali Amendment and EU F-Gas rules.
- Alternative options and challenges: Dry powder inhalers (DPIs) offer up to 98% lower emissions but face barriers like higher costs and entrenched prescribing practices. Patient choice and advocacy are key to wider adoption.
- Future outlook and trade-offs: While low-GWP MDIs and DPIs can drastically cut emissions, concerns remain about cost, clinical suitability and potential indirect warming effects of new propellants. Rapid HFC phase-down could deliver near-term climate benefits.
This summary was generated by AI and checked by a human editor
In 2022, allergist and immunologist Jyothi Tirumalasetty discovered that Stanford Medicine, where she works, had overlooked a big contributor to its climate impact. Metered dose inhalers (MDIs) containing drugs like salbutamol are massively important to people with asthma. Yet, perhaps surprisingly, the propellants used to fire medicine into users’ lungs are powerful greenhouse gases. Emissions from one inhaler, in use for about two months, can be equivalent to those from driving 200 miles in a petrol-powered family car. And those who weren’t aware of this apparently included most of the US healthcare system.
A colleague of Tirumalasetty’s wanted to cut greenhouse gas emissions from MDIs at their hospital, part of a medical system linked to Stanford University in California, US. After he approached Tirumalasetty for help, and she did some research, she remembers telling him ‘We can’t, because we don’t know exactly what our inhaler emissions are here.’ ‘That’s not been included in our carbon footprint analysis for the hospital, and it’s not been included in the one national analysis of the US carbon footprint either,’ she recalls saying.
Thankfully some are aware of inhalers’ climate impact. They include drug companies, who are already developing inhalers with alternative propellants. In May the UK’s drug regulator approved an inhaler for chronic obstructive pulmonary disorder (COPD) from UK-based drug company AstraZeneca. The amount of warming that propellants cause relative to the carbon dioxide we produce from burning fossil fuels is known as their global warming potential (GWP). AstraZeneca uses HFO-1234ze, or trans-1,3,3,3-tetrafluoropropene, which it says has just one-thousandth the GWP of existing propellants.
For the manufacturer of the salbutamol brand Ventolin, UK-headquartered pharma giant GSK, the inhaler is responsible for almost half of its climate impact. The GWP of Ventolin’s current propellant, 1,1,1,2-tetrafluoroethane or HFC-134a, is 1530. Overall MDIs of various brands are responsible for around 3% of the UK National Health Service (NHS)’s climate impact. Therefore GSK is putting a more climate friendly formulation through trials using HFC-152a or 1,1-difluoroethane, whose GWP is one-tenth of that of HFC-134a.
These promising new products should soon be available, but another type of inhaler already exist with a smaller climate impact than current propellants. You could ask your doctor for one – but you might not get it, because they often cost more. Patients can join researchers like Tirumalasetty and campaigning organisations in insisting medical systems offer these green inhalers. But changes needed to avoid the worst gases for the climate are ultimately driven by governments and laws. And unlike many other climate issues, there is a past example of success to build on.
From ozone depletion to global warming
In 1994, University of Manchester respiratory physician Ashley Woodcock received an unexpected phone call from the UK’s then-Department for the Environment. The caller brought up the 1987 Montreal Protocol treaty banning ozone-depleting substances like chlorofluorocarbons (CFCs). ‘“Do you realise that means there’s going to be no inhalers?’” Woodcock recalls the speaker saying. ‘I said “Well, that could be a challenge.”’
CFCs were used for aerosol sprays and coolants for refrigeration, while most MDIs also used CFC-12, or dichlorodifluoromethane as a propellant. Beyond its ozone-depleting chemistry, CFC-12’s GWP is 10,200. Woodcock helped ensure inhalers were temporarily exempt from the ban until companies showed inhalers using hydrofluorocarbon (HFC) alternatives like HFC-134a and HFC-227ea, also known as 1,1,1,2,3,3,3-heptafluoropropane, were safe and effective. ‘The Montreal Protocol is a major success,’ he says. ‘It saved the ozone layer and also probably prevented about one degree of climate change’
HFCs’ warming effect came into focus in 2014. ‘We realised we had solved the ozone depletion issue but still had a climate issue because the increasing use of HFCs, especially in refrigeration and air conditioning, will exacerbate global warming. The Intergovernmental Panel for Climate Change (IPCC) passed the parcel and said “We’ve got enough to do on CO2. You guys were good at getting rid of CFCs, can you phase down HFCs?”’
In 2016, governments agreed the Kigali Amendment to the Montreal Protocol, which will phase down all HFCs. The US and Europe are also introducing F-Gas Regulations restricting these substances, phasing down HFCs faster than the Kigali targets. Starting in 2025, in Europe, HFC producers and importers must pay fees of €3 (£2.60) per tonne of carbon dioxide equivalent for an allocated quota of hydrofluorocarbons they can put onto the market. ‘Since half the inhalers in the world are made in Europe, access to pharmaceutical grade HFC is going to get squeezed by 2030,’ Woodcock says. ‘The pharmaceutical companies are moving quickly to develop low GWP MDIs.’
Testing low-GWP alternatives
Two-thirds of the HFC-134a sold for inhaler propellants come from Orbia Fluor & Energy Materials, explains Sheryl Johnson, pharma application development manager at its Chester, UK, site. These substances are useful for propellants in part because they change between liquid and gas at convenient temperatures and pressures. They exist in a liquid state in an inhaler, then expand to a gas when a user presses on the canister to help deliver the drug to the surfaces in users’ lungs. ‘You can have the classic suspension formulations like Ventolin, where you are suspending the API in the liquefied propellant,’ explains Johnson. ‘There you’re looking for very limited solubility. Then there are solution formulations where you want to actively dissolve the API in the propellant.’
Orbia has been planning for the transition away from the current high GWP propellants for over a decade. It chose HFC-152a, doing toxicology studies to prove its safety. HFC-152a ‘has great solvent power, you need less cosolvent in there to get a successful homogeneous solution’, Johnson notes. Orbia is building a new plant in Runcorn specifically to manufacture the propellant, which is due to be operational in mid-2026.
Moving away from HFCs is not as dramatic as the transition from CFCs, comments Laura Clow, medicine development lead at GSK in Stevenage, UK. Then, ‘the difference in propellant created a difference in product performance’, she says. ‘You almost needed to treat that medicine as a completely new product, and that meant running a full efficacy trial.’
For moving Ventolin to HFC-152a, the European Medicines Agency (EMA) requires fewer studies, exploring aspects including the dose needed and how patients absorb, metabolise and excrete the drug, says Clow. However, the US Food and Drug Administration has required extra studies. ‘We’re having to run quite a big clinical programme,’ Clow says. ‘I don’t expect that will be the case for every product. It’s probably because we’re the most advanced using this particular propellant.’ GSK has completed most of these and is now conducting a final safety study. It announced results showing that the HFC-152a version of Ventolin is equivalent to the existing version in October.
As well as substituting one HFC for another, researchers are exploring hydrofluoroolefins (HFOs) such as HFO-1234ze. AstraZeneca uses HFO-1234ze in its recently approved COPD inhaler, Trixeo Aerosphere, which combines three drugs, budesonide, glycopyrronium and formoterol. Following its UK approval, the EMA also gave a positive opinion on its use in July. It will be available to patients in the UK and EU ‘over the coming months’ according to Pablo Panella, AstraZeneca’s senior vice president of global respiratory and immunology.
Though low GWP inhalers are not yet on the market, respiratory drugs look set to remain available after high GWP HFCs are phased out in the UK in 2030. In fact, users could potentially already choose non-MDI inhalers that reduce carbon emissions – but that choice sometimes disappears when those buying the drugs only look at cost.
The dry powder alternative
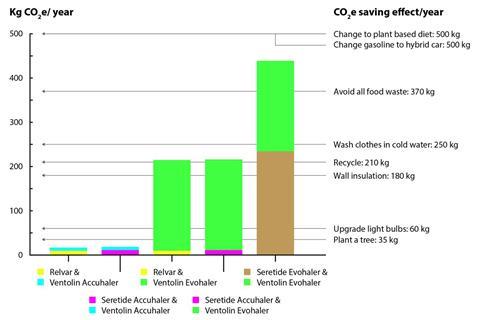
Tirumalasetty and colleagues ultimately filled the gap in knowledge about US emissions from inhalers, assessing the country’s commonly used products. She notes that there is wide variation in inhaler emissions, in part because they vary in size and dosage. They found that lowest emissions come for Proventil, the version of salbutamol produced by Merck & Co, at the equivalent of 10kg of carbon dioxide per inhaler. The emissions from an inhaler of Ventolin itself are equivalent to 29kg of carbon dioxide per inhaler. Two inhalers for mometasone, used to prevent asthma, both produced emissions equivalent to 48kg of carbon dioxide per inhaler. With the average combustion engine car in the UK emitting 200g of carbon dioxide per mile, that equates to 240 miles of driving.
Many within healthcare are unaware of these options to help the environment, Tirumalasetty says. ‘The way our ordering systems are set up in our hospitals, they tend to default to one thing or another,’ she explains. ‘Physicians need to be aware to prescribe lower emissions inhalers.’ Her team is trying to make more people aware and to change ordering systems. ‘They default to higher emission inhalers because that’s preferred by our Medicare/Medicaid insurance.’ Tirumalasetty acknowledges that the decision relates to drug pricing – Proventil costs 50% more than Ventolin, for example.
We need some advocacy to lower those prices
But the most significant environmental improvement in Tirumalasetty’s team’s study comes from swapping to inhalers that don’t use any propellant at all. Called dry powder inhalers (DPIs), they contain mechanical distributors that use a patient’s own inhalation to disperse drug substances. Ventolin itself isn’t available as a DPI in the US. An alternative called ProAir RespiClick, from Teva Pharmaceuticals is responsible for the equivalent of just 0.8kg of carbon emissions per inhaler, the Stanford team estimates.
ProAir RespiClick works out as 25% more expensive than the GSK MDI product in their analysis. Overall costs for DPIs are higher, she concedes, but she believes that this relates little to the actual drug and inhaler costs. Instead, it’s more due to the outcome of negotiations between the US government and drug companies. ‘We need some advocacy to lower those prices,’ she says.
Inhalers are generally excellent value, notes Woodcock. ‘A blue inhaler comes in at 1p per puff,’ he says. ‘There’s no other treatment in the world that costs 1p a go.’ Some generic versions of HFC-134a MDIs are reducing costs by about 20%, he says, and authorities and doctors are switching to them from DPIs based on cost alone.
Yet Woodcock prescribes DPIs for most patients. He considers them to be easier to use, though he concedes that a very few patients may not have enough lung strength to activate DPIs. And he considers MDIs and DPIs to be therapeutically equivalent. However, UK doctors prescribe MDIs to 70% of patients, compared to 13% of patients in Sweden, with the rest using DPIs. ‘It’s all about culture and practice,’ Woodcock adds.
When Woodcock tells patients emissions from current inhalers equate to 200 miles in a family car they say ‘Right, give me a powder inhaler now,’ he reveals. ‘A UK survey showed 80% of patients want an environmentally friendly inhaler. But I accept the fact that many patients like an MDI. We need patient choice, and that will be fine when those MDIs have low environmental impact.’
Whereas HFC-152a reduces MDIs’ climate impact by 93%, the DPI reduction is up to 98%, Woodcock stresses. Inhalers using HFO-1234ze, adopted by AstraZeneca in Trixeo Aerosphere, could get close to this minimal impact of DPIs. But laboratory findings have suggested such hydrofluoroolefins (HFO) could drive warming more potently.
Patient choice versus environmental impact
Max McGillen from CNRS in Orléans, France, started with a simple thought experiment about HFOs. He knew that ozone could react with and break down molecules containing double bonds. HFOs contain double bonds, he reasoned, so could they break down to form HFCs? McGillen decided to look closer at this question, focusing on HFOs that could produce ‘specifically bad HFCs’ he tells Chemistry World.
McGillen and colleagues found in laboratory studies that through ozonolysis HFO-1234ze produced fluoroform, also known as HFC-23, increasing its overall GWP from nearly zero to around 10 and calling into question its green reputation. Though that’s higher than had been thought for HFO-1234ze, it’s still lower than HFC-152a’s GWP. McGillen is ‘confident that these reactions occur in the atmosphere’. ‘Our models of the atmosphere are quite realistic,’ he says. He’s spoken to people from ‘various major fluorochemical companies’ about the process. ‘They are generally interested to know how it works and what this might mean for their products,’ McGillen says.
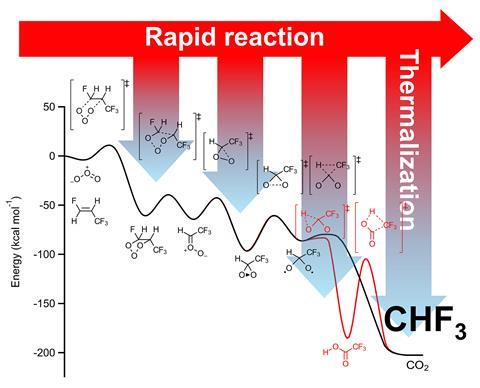
But AstraZeneca won’t be revising its claims for Trixeo Aerosphere’s climate impact based on these findings. Panella says that it has demonstrated that HFO-1234ze has a GWP ‘that is 99.9% lower than currently used propellants’. That’s from a calculation based on ‘internationally accepted’ direct GWP values used in the IPCC’s sixth assessment report (AR6). ‘The McGillen paper employs an alternate approach that differs from that used by the internationally recognised IPCC AR6,’ says Stefan Platz, senior vice president of clinical pharmacology and safety sciences at AstraZeneca. The IPCC’s sixth assessment report doesn’t use such indirect GWP figures, he says. ‘AstraZeneca will always report in line with the internationally accepted standard as provided by the IPCC.’
Panella also notes that in the case of this product, at least, improved climate impact won’t be more costly. ‘There will be no changes to price,’ he says. ‘Reimbursement will not be affected by the introduction of Trixeo with the next-generation propellant versus the outgoing propellant.’
As the ‘green’ version of Ventolin hasn’t yet been approved, it’s too soon for GSK to talk about prices. ‘Negotiations will occur as part of the reimbursement process,’ Clow says. She also stresses that sustainability is part of a ‘trust agenda’ for the company, into which it has invested £1 billion. That includes reviewing its supply chains to reduce their climate impact.
Ventolin offers the biggest opportunity for GSK to improve its climate impact, Clow stresses. ‘If we were to change one single thing, it would be this particular medicine,’ she says. However Clow also emphasises that the European F-gas fees impact the company, which will manufacture its low carbon Ventolin product in Evreux, France.
‘The main driver here is obviously environmental regulation,’ observes Orbia’s Johnson. Her company will therefore continue to supply HFC-134a for MDIs, which the Kigali Protocol allows the continued but reduced use of, for ‘as long as the industry needs it’.
Even as HFC-propelled inhalers transition, physicians like Tirumalasetty and organisations like the Commonwealth Fund are urging policymakers, health care systems and industry leaders to explore lower emission inhalers like DPIs. This provides an opportunity for individuals and other organisations to help drive this transformation, by encouraging doctors to prescribe DPIs. ‘It’s really so critical, given emissions are at their highest ever,’ Tirumalasetty says.
AstraZeneca’s Panella however notes that Trixeo Aerosphere is not available as a DPI. He also highlights that a non-profit called the Respiratory Effectiveness Group says that inhaler choice should balance patient needs and environmental concerns. ‘We strongly oppose switching an inhaler for nonmedical reasons without considering possible clinical consequences,’ the group has written.
Woodcock ultimately points out that there is an upside to HFCs’ greenhouse gas properties, when it comes to phasing them down. As well as being potent, they last for a fairly short time in the atmosphere. ‘HFC 134a, for example, has an atmospheric lifetime of 13 years,’ he explains. The climate impact of HFCs happens in the very near term. ‘If we can phase down HFCs quickly we can achieve most of that benefit in the next decade,’ Woodcock says. ‘Let me tell you, we need that climate benefit right now.’
Andy Extance is a science writer based in Exeter, UK


















1 Reader's comment