Firms anticipate long-term markets for prevention and treatment
Sars-CoV-2 continues to infect millions of people worldwide and cause an estimated 10,000 deaths per day, as the US alone approaches one million dead. It is widely expected to become endemic, remaining in circulation for the foreseeable future, and continuing to cause substantial numbers of hospitalisations and deaths, especially among vulnerable groups. ‘Covid kills about tenfold more people than flu, based on historical information,’ says Penny Ward, professor of pharmaceutical medicine at King’s College London, UK.
Existing vaccines reduce the probability of severe disease, but do not protect against infection. Immunity also wanes within months, particularly against the newest emerging variants. This leaves room for companies to develop more effective antivirals and vaccines in the coming months or even years.
Action on antivirals
There are now three drugs to fight the virus directly: two taken orally and one intravenous. Pfizer’s Paxlovid (nirmatrelvir/ritonavir) inhibits a viral protease enzyme, and the tablets can reduce hospitalisation and death by around 60% when taken early. Lagevrio (molnupiravir), from Merck & Co and Ridgeback Therapeutics, mimics an RNA building block and introduces catastrophic errors in viral RNA. It can cut the risk of hospitalisation or death by around 30%.
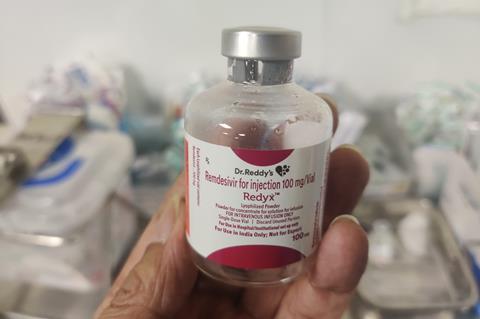
But both have issues. Paxlovid includes ritonavir, which has pharmacogenetic boosting effects, notes Ward, but is incompatible with medications for heart disease, diabetes and other conditions. Molnupiravir cannot be given to pregnant women or children. ‘They’re not the perfect antivirals,’ says Ward. While the third option – Gilead’s Veklury (remdesivir) – might lower the risk of hospitalisation or death by 87%, it must be given intravenously. That leaves plenty of scope for new antivirals. ‘Mortality following hospital admission is between 25 and 40%, depending on the frailty of the individual,’ says Ward. Rapid diagnosis and prescription is also important for the drugs to be effective, which may be problematic as countries cut down access to testing.
There are a few candidate antivirals in development. Atea Pharmaceuticals has a polymerase inhibitor, bemnifosbuvir (AT-537), that it continues to pursue, despite a setback with a phase 2 trial with mild-to-moderate patients that brought a collaboration with Roche to an end in October. ‘They are rejigging the trial design and continuing with development,’ says Ward. Meanwhile, Japanese biotech Shionogi has a protease inhibitor (S-217622) in phase 2a trials.
I think omicron is going to carry us from pandemic to endemic, but we don’t know how much pathogenicity an endemic Sars-CoV-2 will carry
Since antivirals target internal proteins, which do not mutate as much as the spike protein targeted by antibodies, they are expected to hold up well against new variants, and possibly even other coronaviruses. Ward expects strong demand for effective antivirals, to the point where governments would stockpile these treatments, in the same way as flu antivirals. This offers a lucrative market for anyone with large quantities of new, improved antivirals. The US government has bought around 3.1 million courses of molnupiravir, for approximately $2.2 billion, for example.
But supply is likely to continue to be an issue. Molnupiravir is formulated as a powder-filled capsule. ‘There are relatively few capsule filling lines and these have lower production than tablet lines,’ says Ward. ‘Presently, neither [Merck nor Pfizer] can produce enough of these drugs to be able to supply the world,’ says Ward. ‘Most governments will retain them for use in the highest risk population.’
Boosting vaccine supplies
Although the mRNA vaccines from Moderna and Pfizer-BioNTech have dominated in wealthy countries, the New York Times vaccine tracker lists 12 fully approved vaccines, 19 in early or limited use, and 38 in phase 3 efficacy trials. And there are good reasons for them to continue. ‘There are significant limitations with the current vaccines,’ says Kingston Mills from Trinity College Dublin in Ireland. ‘They don’t produce sterilising immunity, meaning they don’t prevent infection.’ He notes that antibody levels drop after each dose, although some of the vaccines seem to induce stronger long-term T-cell memory responses. ‘There is room for the development of vaccines that have better local immunity and better immune memory,’ he concludes. He is optimistic that this can be done.
We have vaccines that are very effective against serious disease and stopping people from ending up in hospital and dying, but they aren’t very good at preventing people from getting infected
Some see the initial slow pace of vaccine coverage to poorer regions as an inevitable result of government decisions. The international Covax initiative to distribute vaccines to lower income countries has faced a barrage of broken promises, delays and logistical difficulties. ‘All policy makers cared about was speed and innovation,’ says Peter Hotez, vaccinologist at Baylor College of Medicine in Houston, US. ‘They got what they paid for: interesting vaccines for smaller populations in the northern hemisphere.’ Early vaccine shipments went to those willing to pay top dollar. But leaving parts of the world unvaccinated has proven risky. Hotez points to the delta and omicron variants both coming out of unvaccinated populations in India and southern Africa, respectively.

Hotez began a coronavirus vaccine programme almost a decade ago, first for Severe Acute Respiratory Syndrome (Sars) after 2012 and then for Middle East Respiratory Syndrome (Mers). When Covid-19 came along, he was ready to develop a vaccine based on the receptor binding domain on the spike. This recombinant protein plus adjuvant vaccine (Corbevax) was licensed to the Indian company Biological E in 2020, and later showed 90% efficacy in phase 3 trials, gaining emergency authorisation in India in late December 2021. It relies on standard yeast fermentation to make its recombinant protein. ‘The technology is similar to that used to make recombinant hepatitis B vaccine,’ says Hotez, meaning it can be made locally in countries such as India, Bangladesh, Vietnam and Brazil. There are no patents, no strings attached, with ownership transferred to the development country vaccine manufacturer. It should be easier to store than mRNA vaccines and, being an older technology, perhaps reassure people hesitant about newer vaccines, he adds.
Other protein-based vaccines are making progress, with Novavax the first to gain approval. Sanofi and GSK began a phase 3 study of their recombinant protein vaccine last summer, announcing preliminary booster results in December and intention to file for regulatory approval this February. Recombinant protein vaccines have different manufacturing requirements than the viral vector, mRNA or live attenuated viral vaccines, which broadens the range of manufacturing facilities available to make more vaccines.
Expanding the options
Other vaccine developers remain confident that their candidates have advantages that will earn them a place in the Covid-19 vaccine market. Canadian company Medicago is growing vaccines in Nicotiana benthamiana – a close relative of tobacco. Young plants are inoculated with a modified agrobacterium that induces them to produce the Sars-CoV-2 spike protein. After a few weeks, the plants are processed to harvest virus-like particles from the leaves. ‘They are the same shape, size and exterior appearance as the native virus, which is one of the reasons we think they are so immunogenic,’ says Brian Ward, medical officer at the company. The finished vaccine, dubbed Covifenz, also includes GlaxoSmithKline’s immune response-boosting adjuvant ASO3.
In trials, Covifenz was around 70% effective against the delta variant in December 2021, and was approved in late February by Health Canada. Medicago sees much of its sales in the booster market and is shortly starting a trial in patients who already received other approved vaccines. However, the World Health Organization decided against accepting it for emergency use, owing to the company’s links to the tobacco industry – Medicago is 33% owned by Philip Morris International.
If we want to prevent symptomatic disease, then we will have to give boosters very frequently, six-monthly or perhaps even three-monthly
Other companies are also targeting boosters. US biotech firm Arcturus Therapeutics has developed an mRNA vaccine (ARCT-021) that is self-amplifying. Whereas the mRNA in approved Covid-19 vaccines makes spike protein for a day or two, Arcturus’ mRNA churns out spike for one to two weeks. Chief executive Joseph Payne explains that this means the dose can be significantly reduced, to 5µg per dose, compared to 30µg for Pfizer–BioNTech and 50µg for Moderna.
A lower dose means less RNA is injected, meaning less of the other ingredients in the formulation as well. ‘The key side effects with vaccines are attributed not to the mRNA but to the [other] ingredients,’ says Payne, so he hopes to see a more attractive safety profile. Also, production should stretch much further, in theory allowing the firm to manufacture more doses at lower cost than other mRNA vaccines. Arcturus has manufacturing agreements in place in the US, Japan and Europe, and is building a production facility in Hanoi, Vietnam. In late April, the company reported 95% efficacy in preventing severe Covid-19 in trials in Vietnam, and 55% efficacy in preventing symptomatic illness.
‘We have vaccines that continue to be very effective against serious disease and stopping people from ending up in hospital on ventilators and dying,’ says Adam Finn, immunologist at the University of Bristol, UK. ‘But they aren’t very good at preventing people from getting infected.’ Meanwhile, Moderna and Pfizer and other vaccine companies have developed omicron-specific boosters, but it remains to be seen if these will be effective or necessary. Finn says current vaccines are tuned to the wrong virus, ‘but you could rush to make a vaccine based on the latest variant, and by the time you’ve manufactured it, it is no longer the relevant variant’. It might be that vaccines covering multiple variants will eventually be rolled out.
Long-term prognosis
Immunologists view mixing of vaccines favourably, with the European Medicines Agency noting that combining mRNA and viral vector vaccines produces good levels of antibodies and a higher T-cell response. ‘A booster with another platform will get a better response,’ says Mills.
Kings College’s Penny Ward agrees: ‘If we want to prevent symptomatic disease, then we will have to give boosters very frequently, six-monthly or perhaps even three-monthly.’ She views vaccines at a more efficient way to manage the disease than relying on more expensive antivirals.
Nonetheless, there is some opposition to the idea of continuing to boost significant numbers of people. ‘This is not a tenable path,’ says Steve Brozak, biotech analyst. ‘The speed of omicron was too fast. We can develop a prototype vaccine, but by the time you actually manufacture it, you’re probably three quarters through the infection peak.’ Even in most wealthy countries, it will not be feasible to continue vaccinating the entire population at regular intervals. ‘Instead of dealing with the virus, deal with the damage it does,’ Brozak suggests, for example using the cheap steroid, dexamethasone, which can reduce mortality in the severely ill. There are multiple efforts to dampen inflammation in severe Covid-19 with novel drugs.
Paul Offit, a vaccinologist at Children’s Hospital of Philadelphia, US, believes that boosters for young adults are not risk free and that vaccines were never meant to protect against infections or mild illnesses. Offit says that two or three doses of vaccine should suffice for most people. ‘Immunisation can protect against severe disease for a long time,’ he says. He is critical of vaccine companies alluding to yearly vaccines, since ‘there’s no evidence for that yet’.
The eventual fate of the Sars-CoV-2 virus remains uncertain. There is a strong suspicion that it will follow a path towards becoming a ‘common cold’ coronavirus, although how long it would take to reach this destination is unknown. ‘It might become a regular human endemic coronavirus over the next eight to ten years,’ says Penny Ward, ‘and I think omicron is going to carry us from pandemic to endemic, but we don’t know how much pathogenicity an endemic Sars-CoV-2 will carry with it.’
Regular boosters of vulnerable groups may be needed for years to come to protect against severe disease, with Covid-19 sticking around to cause cold symptoms amongst healthy adults and severe illness among vulnerable people. Treatments for vulnerable patients will continue to be needed, especially in countries where vaccination and/or infection rates have been relatively low.
















No comments yet